Ankle Syndesmosis Injuries
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
High ankle sprains or syndesmotic ankle sprains are less common than other ankle pathologies. Athletes may experience it more frequently after forced external rotation and dorsiflexion of the foot. Injuries to the bones and ligaments of the ankle are associated with ankle syndesmosis injury. While surgical intervention is rarely indicated in the absence of fracture, conservative physiotherapy management can aid in a faster recovery. A good understanding of the structures, functional anatomy, and etiologic factors in syndesmosis ankle injuries is needed to treat this injury effectively.
This article discusses the assessment and interventions for grade 1 and 2 syndesmotic ankle sprain.
Definition[edit | edit source]
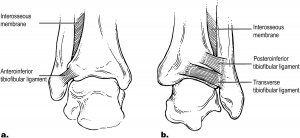
A syndesmosis is "a joint where two bones are held together by ligaments."[1] The distal tibiofibular syndesmosis is formed by two bones, the concave tibia and convex fibula, and four ligaments.[2] The ligaments that link the bones are the distal anterior inferior tibiofibular ligament, the distal posterior inferior tibiofibular ligament, the transverse ligament and the interosseous ligament.[2] No clear definition of the boundaries for the ankle syndesmosis is available. However, according to Kelikan and Kelikan,[3] the boundaries of the distal tibiofibular joint are the origin of the tibiofibular ligaments on the tibia and their insertion into the fibular malleolus.[2]
Clinically Relevant Anatomy[edit | edit source]
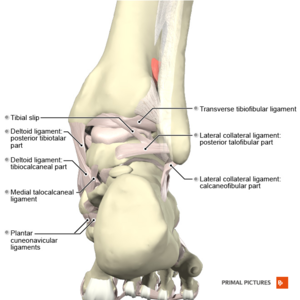
The anterior tubercle of the tibia makes up the anterior margin of the syndesmosis joint, while the posterior tubercle creates its posterior margin. Because the anterior tibial tubercle is more prominent than the posterior tubercle, it stops the distal fibula from slipping forward. The tibia and fibula have complete contact at the base of the syndesmosis. This area, called the tibiofibular contact zone, is covered by 0.5-1 mm thick hyaline cartilage. A synovial recess is present between the distal tibia and fibula and is at risk of tearing in an acute injury. This would affect the anterior tibiofibular ligament.[2]
Superficially located, the anterior inferior tibiofibular ligament is the weakest link of the four ligaments that make up the distal tibiofibular syndesmosis. It cannot overcome the fibula's external rotation forces.[2]
The strong posterior inferior tibiofibular ligament runs from the posterior tibial malleolus to the posterior tubercle of the fibula.[2] Excessive supination-eversion, pronation-eversion or pronation-abduction can cause this ligament to rupture, or (more frequently), a posterior malleolus avulsion fracture can occur.
The transverse ligament extends between the proximal margin of the fibular malleolar fossa and the dorso-distal rim of the tibia. It can run as far as the dorsal aspect of the medial malleolus.[2] Its role is similar to the labrum in the shoulder as it deepens the posteroinferior rim of the tibia.
The interosseous membrane extends between the tibia and fibula and it gradually transitions into a ligament. Not every individual has this ligament. In some cases, it is absent, while in others, it has a strong presence. The interosseous ligament is called a spring ligament for its action of separating the medial and lateral malleolus during dorsiflexion at the talocrural joint. It allows a downward movement of the fibula under load.[4]
In summary, the ligaments that stabilise the inferior tibiofibular syndesmosis:
- Prevent excess fibular motion in multiple directions, including anterior-posterior and lateral translation, craniocaudal translation, and internal and external rotation[5]
- Provide strong opposition of the tibia to the fibular notch of the tibia[4]
- Limit widening of the ankle mortise under full body weight to a maximum of 1 mm. According to Harris and Fallat,[6] "widening of the ankle mortise by 1 mm decreases the contact area of the tibiotalar joint by 42%", leading to joint instability[6]
- Allow the fibular to rotate 3-5 degrees in ankle dorsiflexion and platarflexion[4]
Syndesmosis Injury / Pathological Process[edit | edit source]
The long-term consequence of an ankle sprain is ankle instability; instability remains a problem for 40% of patients. 8% of all lateral ankle sprains lead to distal tibiofibular syndesmosis injury.[4] Joint fractures can be associated with syndesmosis injuries. Syndesmotic injuries frequently happen during the following movements:[4]
- The foot is in a fixed position, and the ankle is in dorsiflexion—motion: external rotation of the foot while the tibia rotates internally.
- The foot is in a fixed position, and the ankle is in dorsiflexion—motion: internal rotation of the foot while the tibia rotates externally.
- Running and jumping sports during which the player's foot stops, and they fall forwards.
A patient with syndesmosis injury usually presents with:[4]
- All around ankle swelling
- Pain localised to the anterior inferior tibiofibular ligament during active and passive external rotation of the foot and forced dorsiflexion.
- Heel-raise gait to avoid pain on push-off
- Haematoma along the tibia
Classification of Syndesmosis Sprains[edit | edit source]
Chronological classification:[7]
- Acute (within the first three weeks of injury)
- Subacute (three weeks to three months)
- Chronic (beyond three months)
West Point Ankle Grading System:[4][7]
- The system considers the degree of instability, ability to bear weight, the extent of oedema, the localisation of tenderness, response to provocative stress tests, and evidence of radiographic widening.
- Grade 1: mild, no instability. Squeeze and external rotation tests are negative. The patient might or might not have some bruising anterior to the joint and maybe up along the shin.
- Grade 2: moderate, some evidence of instability. Squeeze and external rotation tests are positive—patient complaints of severe pain and inability to walk. Severe swelling is present in the lower leg, often along the peroneal muscle bellies. Presence of anterior bruising.
- Grade 3: definite instability and positive X-rays (reduced overlap, apparent widening). Presence of a fracture.
Diagnostic Procedures/Special Tests[edit | edit source]
Diagnostic Procedures[edit | edit source]
Conventional radiograph:
- Anteroposterior (AP) and mortise views
- The three most commonly used techniques to evaluate this injury are: tibiofibular clear space (TFCS), the tibiofibular overlap (TFO), and the clear medial space (MCS). The normal tibiofibular area is more than 6 mm in AP view and more than 1 mm in mortise view
- According to Krähenbühl et al.,[8] a conventional radiograph is not reliable in predicting syndesmotic injuries
- Based on the findings of Chun et al.,[9] simple radiography has reasonable specificity
CT scan:
- The tibiofibular width (axial images) is most commonly used
- More sensitive to detect positional faults (tibia and fibula)
- Allows for a detailed assessment of the syndesmotic interval
- Based on a systematic review by Chun et al.,[9] CT scans have "high sensitivity and specificity irrespective of accompanying fracture"[9]
- A weight-bearing CT should be performed if the patient can support weight on their foot[10]
- According to Malhotra et al.,[11] a weight-bearing CT helps in the functional assessment of syndesmosis injuries
Diagnostic Ultrasound
- Able to detect syndesmosis injury at ≥6.0 mm of tibiofibular clear space widening[12]
MRI
- Obtained measurements achieve a sensitivity and specificity of nearly 100%[8]
- Similar accuracy to gold standard arthroscopic findings[9]
- Can detect associated soft tissue injuries and osteochondral lesions[4]
Special Tests[edit | edit source]
- Squeeze Test
- Performed by squeezing the tibia and fibula together above the injury
- It helps to assess the integrity of the interosseous membrane and syndesmotic ligaments
- In the presence of a fibular fracture, pain appears along the fibular shaft
- In syndesmosis injuries, pain appears along the distal tibiofibular joint
- Dorsiflexion Compression Test
- The ankle is in maximal dorsiflexion and the patient is weight bearing. Medial-lateral compression is applied.
- This test is positive when there is a decrease in pain on dorsiflexion or an increase in the dorsiflexion range.
Management / Intervention[edit | edit source]
General Principles[edit | edit source]
Limited resources are available to guide the treatment of syndesmosis injuries. It is important to consider the following:[4]
- Apply caution because you are treating an unstable structure
- Follow the same principles as in rehabilitation for chronic ankle instability:
- Avoid inversion and eversion early on
- Avoid extreme dorsiflexion
- Avoid extreme plantarflexion during the first two weeks
- Restrict weight bearing to non-weight bearing with crutches for one to three weeks
- Progress to full weight bearing within four to six weeks
- Start with a foam walker or a boot and progress to a brace as pain subsides
- Monitor pain and proceed according to the patient's pain
- Avoid too much pronation when starting load-bearing rehabilitation
Grade 1 and Grade 2[edit | edit source]
Conservative management should be used for individuals with Grades 1 and 2 injuries based on the West Point Ankle Grading System. The patient may require six to eight weeks of rehabilitation. The following interventions and education strategies are recommended:[4]
- Determine the integrity of the medial ligament. In the case of a torn ligament, the outcome is generally poor.
- More than ten days of immobilisation is required. Instruct on non-weigh-bearing gait for up to three weeks and progress according to pain.
- Start functional mobilisation using an ankle-foot-orthosis (AFO) or semi-rigid brace.
- Use of heel lift for walking to decrease push off.
- Exercise examples:
- Sitting on a Pezzi (Swiss) ball and performing upper body exercises: Sit on a Swiss ball, hold a medicine ball or a dumbbell with your hands. Draw your belly button inwards to contract the abdominal muscles, and keeping the arms straight, pull the dumbbell or medicine ball across your body so the dumbbell ends above your opposite shoulder.
- Sitting on a Pezzi (Swiss) ball and moving forwards and backwards: Sit on a Swiss ball and draw your belly button inwards to contract the abdominal muscles. Roll the ball by tilting your pelvis backwards and forward.
- Bridging on the ball: Lie flat on the back, with knees flexed and feet resting on a Swiss ball. Both arms are down with palms facing down. Once your feet are stable on the ball, squeeze your bottom muscles, lift your buttocks and lower back in the air. Ensure to maintain good posture and contract the deep abdominal muscles by squeezing the abdomen towards the spine.
Grade 2[edit | edit source]
- Return to the sport will be possible after 6 – 8 months
- Repeated MRI is recommended within six weeks or less if there is no improvement with conservative treatment
- Referral to a specialist may be required if the syndesmosis is not mechanically stable and if surgery is required
- For post-surgical management, the patient must maintain partial weight bearing for six to eight weeks after surgery
Resources[edit | edit source]
- Hermans JJ, Beumer A, de Jong TA, Kleinrensink GJ. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat. 2010 Dec;217(6):633-45.
References[edit | edit source]
- ↑ Cambridge Advanced Learner's Dictionary & Thesaurus. Cambridge University Press [last accessed 8.08.2022]. Available from https://dictionary.cambridge.org/dictionary/english/syndesmosis
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Hermans JJ, Beumer A, de Jong TA, Kleinrensink GJ. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat. 2010 Dec;217(6):633-45.
- ↑ Kelikian H, Kelikian S. Disorders of the Ankle.Philadelphia: W.B. Saunders Company; 1985. pp. 4–8.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 Simpson H. Ankle Syndesmosis Injury Course. Physiopedia 2022
- ↑ Anand Prakash A. Anatomy of Ankle Syndesmotic Ligaments: A Systematic Review of Cadaveric Studies. Foot Ankle Spec. 2020 Aug;13(4):341-350.
- ↑ 6.0 6.1 Harris J, Fallat L. Effects of isolated Weber B fibular fractures on the tibiotalar contact area. J Foot Ankle Surg. 2004 Jan-Feb;43(1):3-9.
- ↑ 7.0 7.1 Del Buono A, Florio A, Boccanera MS, Maffulli N. Syndesmosis injuries of the ankle. Curr Rev Musculoskelet Med. 2013 Dec;6(4):313-9.
- ↑ 8.0 8.1 Krähenbühl N, Weinberg MW, Davidson NP, Mills MK, Hintermann B, Saltzman CL, Barg A. Imaging in syndesmotic injury: a systematic literature review. Skeletal radiology. 2018 May;47(5):631-48.
- ↑ 9.0 9.1 9.2 9.3 Chun DI, Cho JH, Min TH, Yi Y, Park SY, Kim KH, Kim JH, Won SH. Diagnostic accuracy of radiologic methods for ankle syndesmosis injury: a systematic review and meta-analysis. Journal of Clinical Medicine. 2019 Jul 3;8(7):968.
- ↑ de Albornoz PM, Monteagudo M. Pathomechanics of Syndesmotic Injuries. Journal of Foot and Ankle Surgery (Asia Pacific). 2021 Oct 20;8(4):163.
- ↑ Malhotra K, Welck M, Cullen N, Singh D, Goldberg AJ. The effects of weight bearing on the distal tibiofibular syndesmosis: A study comparing weight bearing-CT with conventional CT. Foot Ankle Surg. 2019 Aug;25(4):511-516.
- ↑ Fisher CL, Rabbani T, Johnson K, Reeves R, Wood A. Diagnostic capability of dynamic ultrasound evaluation of supination-external rotation ankle injuries: a cadaveric study. BMC Musculoskelet Disord. 2019 Oct 30;20(1):502.
- ↑ Molinari A, Stolley M, Amendola A. High ankle sprains (syndesmotic) in athletes: diagnostic challenges and review of the literature. Iowa Orthop J. 2009;29:130-8.
- ↑ Russ Hoff. Kleiger's Test or External Rotation Test. Available from: https://www.youtube.com/watch?v=LnB1fta_rQA [last accessed 11/08/2022]
- ↑ PTP621 2014. Squeeze Test (Foot/Ankle). 2015 Available from: https://www.youtube.com/watch?v=fAy8BVy6QTQ [last accessed 11/08/2022]
- ↑ CRTechnologies. Dorsiflexion Compression Test (CR). 2011 Available from: https://www.youtube.com/watch?v=GnRVUOQF7mA [last accessed 11/08/2022]