Acute Lymphoblastic Leukemia
Original Editors - Erin Foster from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Erin Foster, Admin, Lucinda hampton, Kim Jackson, Elaine Lonnemann, WikiSysop, Vidya Acharya, Evan Thomas, Sarah Haerinck, Fasuba Ayobami, 127.0.0.1 and Wendy Walker
Definition/Description[1][2][3][4]
[edit | edit source]
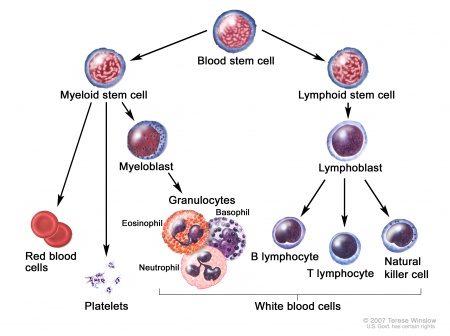
Acute lymphoblastic leukemia (ALL) is a cancer of the blood and bone marrow. Bone marrow is spongy tissue that fills the cavity of the long bones consisting of fat, red blood cells, and white blood cells. ALL affects the immature white blood cells. This type of cancer is classified by one of two subtypes.
[Photo courtesy of The University of Chicago Medical Center. Available at http://www.uchospitals.edu/online-library/content=CDR257989]
The two subtypes include:
B-cell- produce antibodies to fight infections.
- Common ALL (50% of cases)
- Early Pre-B ALL (10% of cases)
- Pre-B ALL (10% of cases)
- Mature B-cell ALL (4% of cases)
T-cell- assist B-cells in producing antibodies to fight infections.
- Pre-T ALL (5-10% of cases)
- Mature T-cell (15-20% of cases)
Prognostic factors include:[5] [6]
- Age: Younger patients have a better prognosis compared to older patients. The cure rate of children is approximately 80% and only 40% for adults.
- Initial white blood cell (WBC) count: Patients diagnosed with a WBC count below 50,000 tend to do better than patients with higher WBC counts.
- ALL subtype: The subtype of T cell or B cell affects prognosis. Patients with T-cell ALL tend to have a better prognosis than those with mature B-cell ALL.
- Response to chemotherapy: Patients who achieve complete remission within 4 to 5 weeks of starting treatment tend to have a better prognosis. Patients who do not achieve remission at any time have a poor prognosis. Evidence of minimal presence of leukemia cells in the bone marrow may also positively affect prognosis.
Prevalence[2]
[edit | edit source]
ALL is the most common cancer occurring in children today and can occur in some adult cases. Children are at the highest risk between 2 and 4 years of age. This risk decreases from age 4 to mid-20s, increasing again after age 50. The average person has a 1 in 1,000 chance of getting ALL. The American Cancer Society estimated the following statistics for 2010:
- Approximately 43,050 new cases of all types of leukemia.
- Approximately 5,330 new cases of acute lymphoblastic leukemia (1 out of 3 were adult cases).
- Approximately 1,420 deaths from ALL (3 out of 4 were adult cases).
Characteristics/Clinical Presentation[1][3][4][edit | edit source]
Most signs and symptoms of ALL mimic those of the flu. However, with ALL these signs and symptoms will not improve. Signs and symptoms include:
- Weight loss
- Bleeding from the gums
- Nosebleeds
- Pale skin
- Shortness of breath
- Fever
- Frequent infections
- Weakness
- Fatigue
- Swollen lymph nodes (neck, underarm, groin, stomach)
Red blood cells: These cells carry oxygen throughout the body. A low number of red blood cells can lead to feeling tired or weak, being short of breath and looking pale (anemia).
White blood cells: These cells fight infections. A low number of white blood cells can lead to fever and frequent infections that are hard to treat.
Platelets: Platelets control bleeding. A low number of platelets can lead to slow healing, easy bruising or bleeding and tiny red spots under the skin (petechiae).
Leukemia cells: An increased number of these cells can cause pain in the bones or joints, lack of appetite, headache or vomiting.
Associated Co-morbidities[7] [6][edit | edit source]
The following co-morbidities are linked to ALL:
- Anemia: a deficiency of red blood cells.
- Diabetes: disorder characterized by defects in the body's ability to produce or use insulin resulting in high blood glucose levels.
- Lupus: a chronic autoimmune disease that effects many systems in the body.
- Rheumatoid Arthritis: a chronic systemic inflammatory disorder.
- Multiple Sclerosis: an autoimmune disease that attacks the central nervous system.
Medications[8][edit | edit source]
Medications involved with ALL include:
- Chemotherapy drugs: L-asparaginase, Vincristine
- Steroid: Dexamethasone, Hydrocortisone
- Drugs for high-risk patients: Daunorubicin, Cytarabine
- Other drugs that may be given early: Methotrexate, 6-mercaptopurine.
Diagnostic Tests/Lab Tests/Lab Values[1][4][edit | edit source]
Diagnostic tests and results for ALL include:
Blood test: These tests reveal increased number of white blood cells, decreased number of red blood cells (anemia) and platelets (thrombocytopenia). A blood test may also reveal blast cells. Blast cells are immature blood cells in bone marrow.
[edit | edit source]
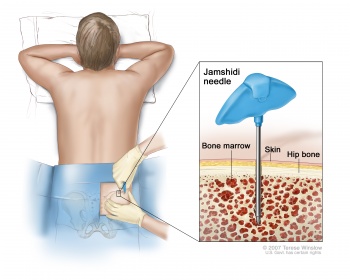
Bone marrow test: A needle is used to remove a sample of bone marrow from the hipbone to look for cancerous cells. Through this process, doctors can determine if the cells originated from the B lymphocytes or T lymphocytes according to certain changes in the cancer cells.
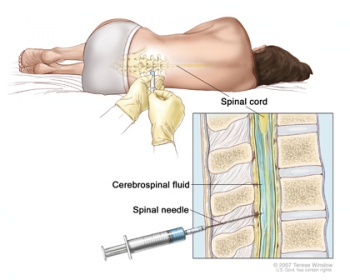
Lumbar puncture or spinal tap: A sample of spinal fluid is collected to determine if the cancerous cells have spread.
Imaging: X-ray and computerized tomography (CT) scan can help determine if the cancer has spread to other parts of the body.
[Photo courtesy of The University of Chicago Medical Center. Available at http://www.uchospitals.edu/online-library/content=CDR257989]
Etiology/Causes[1][2][4][edit | edit source]
The exact causes are unknown. However, there are some risk factors thought to be linked to ALL. These risk factors include:
- Gender- slightly more common in males than females
- Ethnicity- more common in Caucasians
- Chemical exposure or past chemotherapy treatments
- Radiation exposure or past radiation treatments
- Viral infection
- Certain inherited disorders
Down syndrome: The most frequently occurring chromosomal condition occurs when an individual has three copies of the 21st chromosome instead of two. Those with Down syndrome have increased risk for medical conditions such as congenital heart defects, respiratory issues, hearing problems, Alzheimer's disease, childhood leukemia, and thyroid conditions.
Klinefelter syndrome: The most common sex chromosome disorder in males. This syndrome occurs when an extra X chromosome is present affects sexual development.
Fanconi anemia: This type of inherited anemia is a very rare, recessive genetic disorder that leads to bone marrow failure.
Bloom syndrome: This syndrome is a very rare inherited genetic disorder caused by a gene that does not function properly causing an unusually high number of breaks or instability along their chromosomes. This instability causes an increased risk to develop many cancers and leukemia at early ages.
Ataxia-telangiectasia: A-T is a genetic progressive disease that affects the immune system occurring in early age.
Neurofibromatosis: A genetic disorder that causes tumors to develop in the nervous system.
Systemic Involvement[edit | edit source]
| Presentation | Cause |
| anemia, pallor, fatigue, malaise, hypoxia, bleeding | rapidly proliferating development of leukocytes inhibiting erythrocytes and thrombocytes |
| severe infections, ulcerations of the mouth and throat | high numbers of immature or abnormal leukocytes unable to fight and destroy microorganisms |
| increased metabolic rate accompanied by weakness, pallor, and weight loss | increased leukocyte production requiring large amounts of nutrients; cell destruction increases the amount of metabolic wastes |
| headache, disorientation | abnormal white cells infiltrating the central nervous system |
| hyperuricemia causing renal pain, obstruction, and infection; a late development is renal insufficiency with uremia | large amounts of uric acid released as a result of destruction of great numbers of leukocytes; in late stages, abnormal leukocytes infiltrate the kidneys |
| enlarged organs exerting pressure on adjacent organs | high numbers of white cells accumulating within the liver and spleen, causing distention of tissue |
| lymphadenopathy and bone pain | excessive numbers of white cells accumulating in lymph nodes and bone marrow |
[Information with photo found in Pathology: Implications for Physical Therapists][6]
Anemia: deficiency of red blood cells
Pallor: deficiency of color, especially in the face
Malaise: feeling of fatigue and discomfort
Hypoxia: oxygen deficiency
Hyperuricemia: abnormally high level or uric acid
Lymphadenopathy: abnormally enlarged lymph nodes
Medical Management (current best evidence)[1][3][4][8][edit | edit source]
Treatment for ALL can span from 2 ½ to 3 ½ years depending on each individual situation. General treatment for ALL is broken down into the following 4 phases:
1. Induction therapy: The purpose of this phase is to achieve remission by killing most of the cancer cells in the blood and bone marrow. During the first month, the patient may require many doctor's visits due to increase risk of infections. Patients often receive 3 drugs for the first month of treatment which include:
- Chemotherapy drugs injected intrathecally
- Steroids
- A fourth drug in the anthracycline class is typically added for high-risk patients.
2. Consolidation therapy/ Post- remission therapy: During this more intensive phase, the goal is to destroy any remaining leukemia cells in the central nervous system. This phase of chemotherapy lasts typically 4 to 8 weeks. Intrathecal therapy is continued during this phase.
3. Maintenance therapy: This low dose treatment is given to prevent cancer cell re-growth. During the first few months of this phase, most treatments include 1 to 2 treatments similar to the initial induction. These 4 week intense treatments are called re-induction.
4. Preventive treatment to the spinal cord: Some cancer cells in the central nervous system can not be destroyed by chemotherapy drugs given by oral or intravenous means. During this phase, chemotherapy drugs are injected directly into the spinal cord fluid.
During these 4 phases the specific types of treatments include:
Chemotherapy: Chemotherapy is normally used in the induction therapy stage to kill the cancer cells. This drug can also be used in the consolidation and maintenance phases. All patients need spinal taps to inject chemotherapy into the cerebrospinal fluid (CSF) to kill any leukemia cells that may have spread to the brain and spinal cord. This intrathecal chemotherapy is usually given twice during the first month and four to six times during the next one to two months. It is repeated less often during the rest of consolidation and maintenance. A possible side effect of intrathecal chemotherapy is epileptic seizures during treatment.
Chemotherapy can be received several ways:[9]
- Orally
- Intravenous injections
- Catheter placement involving a tube placed in a large vein for patients that require many IV treatments
- Intrathecal injections into the cerebral spinal fluid or through a catheter placed under the scalp
Targeted drug therapy: These drugs attack specific abnormalities that cause the cancer cell growth.
Radiation therapy: This treatment uses high-powered beams to destroy cancer cells. This is typically used when the cancer has spread to the central nervous system. Along with intrathecal chemotherapy, high-risk patients and those with leukemia cells detected in their CSF may be given radiation therapy to the brain and spinal cord. Doctors try to avoid this treatment if possible, especially in younger children, because it may cause problems in growth and development.
Stem cell transplant: This transplant may be used for patients at risk or currently going through a relapse. This procedure replaces cancer bone marrow through chemotherapy or radiation with healthy bone marrow from a compatible donor allowing re-establishment of healthy stem cells.
Physical Therapy Management (current best evidence)[edit | edit source]
Practice Pattern: The practice patterns are determined on an individual basis depending on clinical presentation and response to medical intervention.[6]
| Area of Focus | Intervention | Frequency |
| Pain |
Modalities |
As needed |
| Strengthening |
Therapeutic exercise |
3-5 days a week |
| Stretching |
Continuous passive motion machine |
1-5 times a week |
| Endurance |
Walking |
5 times a week |
| Manual Techniques |
Manual guidance |
As needed |
| Motor learning principles |
Knowledge of performance |
As needed |
[Information and table found in Pediatric Physical Therapy][10]
Precautions should be taken for:[6]
- Thrombocytopenia: low number of platelet
- Neutropenia: low number of neutrophils (WBC)
- Infection control: signs of infection include mucosal ulceration, skin abrasion, or other tears
- Anemia
- Medication side effect
- Drug induced mood changes
Differential Diagnosis[edit | edit source]
The following are possible differential diagnosis for ALL:
- Acute myelocytic leukemia
- Acute anemia
- Juvenile Rheumatoid Arthritis
- Leukocytosis
- Mononucleosis and Epstein-Barr virus
- Neuroblastoma
- Non-Hodgkin Lymphoma
- Osteomyelitis
- Parvovirus B19 infection
- Rhabdomyosarcoma
Case Reports/ Case Studies
[edit | edit source]
[Photo courtesy of Medimanage]
- Gohar SF, Marchese V, Comito M. Physician referral frequency for physical therapy in children with acute lymphoblastic leukemia. Pediatr Hemotol Oncol. 2010; 27: 179-87.
- Marchese VG, Chiarello LA, Lange BJ. Effects of physical therapy intervention for children with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2004; 42: 127-33.
- Tecklin J.S. Pediatric Physical Therapy. Lippincott, Williams and Wilkins. Baltimore, Maryland. Fourth Edition. 2008:551-552.
Resources
[edit | edit source]
- American Cancer Society
- National Marrow Donor Program
- Mayo Clinic
- Leukemia & Lymphoma Society
- American Society of Hematology
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=107QS1L1jrY: Error parsing XML for RSS
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Mayo Clinic. Acute Lymphoblastic Leukemia. 2010. Available at: http://www.mayoclinic.com/health/acute-lymphocytic-leukemia/DS00558/TAB=indepth. Accessed March 7, 2011.
- ↑ 2.0 2.1 2.2 American Cancer Society. Leukemia—Acute Lymphocytic Overview. 2010. Available at: http://www.cancer.org/Cancer/Leukemia-AcuteLymphocyticALLinAdults/OverviewGuide/leukemia-all-overview-what-causes. Accessed March 7, 2011.
- ↑ 3.0 3.1 3.2 National Marrow Donor Program. Acute Lymphblastic Leukemia. 2011. Available at: http://www.marrow.org/PATIENT/Undrstnd_Disease_Treat/Lrn_about_Disease/ALL/index.html. Accessed March 7, 2011.
- ↑ 4.0 4.1 4.2 4.3 4.4 The Chicago University Medical Center. Adult Acute Lymphoblastic Leukemia Treatment. 2011. Available at: http://www.uchospitals.edu/online-library/content=CDR257989 . Accessed March 7, 2011.
- ↑ University of Maryland Medical Center. Acute Lymphocytic Leukemia- Prognosis. 2011. Available at: http://www.umm.edu/patiented/articles/how_characteristics_of_acute_lymphocytic_leukemia_cells_prognosis_000086_7.htm . Accessed March 7, 2011.
- ↑ 6.0 6.1 6.2 6.3 6.4 Goodman, C., Boissonault, W. Pathology: Implications for the Physical Therapist. Saunders. Philadelphia, Pennsylvania. Third edition. 2009.
- ↑ Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for referral. Saunders, St. Louis, Missouri. Fourth Edition. 2007.
- ↑ 8.0 8.1 American Cancer Society. Treatment of Children with Acute Lymphocytic Leukemia. 2011. Available at: http://www5.cancer.org/docroot/CRI/content/CRI_2_4_4X_Treatment_of_Children_with_Acute_Lymphocytic_Leukemia_24.asp. Accessed March 7, 2011.
- ↑ MedicineNet. Leukemia. 2011. Available at: http://www.medicinenet.com/leukemia/page5.htm. Accessed April 5, 2011.
- ↑ Tecklin J.S. Pediatric Physical Therapy. Lippincott, Williams and Wilkins. Baltimore, Maryland. Fourth Edition. 2008.