Acromioclavicular Arthritis
Introduction[edit | edit source]
Osteoarthritis is the most common cause of shoulder pain originating from the acromioclavicular (AC) joint. ACJ osteoarthritis is a frequent finding in middle-aged people.[1]
Most of the patients are asymptomatic, and they may present as an incidental finding in shoulder X-Ray or Magnetic resonance imaging (MRI). Pain and dysfunction of ACJ origin may lead to an inability to perform manual labor tasks and sports and difficulty doing overhead and cross-body activities. [2]Functional limitations of ACJ pain include difficulty with resistance-training activities that place the glenohumeral joint in an extended position, common in weightlifters so ACJ arthritis is also known as Weightlifter's Shoulder.[3]
AC joint arthritis is caused due to early degeneration of the cartilage and intraarticular disc. Arthritis is often associated with distal clavicular osteolysis.[2] Damage to the ACJ can be synchronous with damage to the supraspinatus tendon and osteophytes from the arthritic joint may contribute to subacromial impingement exacerbating and producing further shoulder pain.[2]
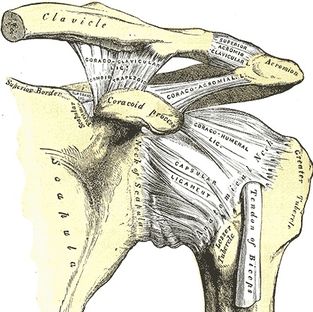
Clinically Relevant Anatomy[edit | edit source]
The ACJ is a synovial joint that provides the scapula with an additional range of rotation on the thorax, which allows the scapula to adjust outside of its initial plane (posterior tipping and internal rotation) to follow the changing shape of the thorax as arm movement occurs.
To learn more about Acromioclavicular joint Click here.
Epidemiology[edit | edit source]
- 12-month prevalence of shoulder pain has been estimated to be 30%, which is second only to low back pain.
- Acromioclavicular joint (ACJ) disease is reported to be present in 31% of all patients with shoulder pain.[3]
- The incidence of ACJ pain is reported to be between 0.5 to 2.9/1000/year in primary care.[2]
- However, the true prevalence is still not clear because most of the time arthritic changes go on silently without producing any symptoms which makes diagnosis more difficult.[4]
- It is common in middle-aged people.[1]
Etiology[edit | edit source]
Type of AC joint arthritis-Based on the etiology
- Primary osteoarthritis: It is articular degeneration without any apparent underlying cause. It more commonly affects the AC joint than a glenohumeral joint. It develops as a consequence of constant stress on the joints, often in people who perform repeated overhead lifting activities.
- Secondary osteoarthritis: It is due to other associated causes like post-trauma or other underlying diseases such as rheumatoid arthritis. Post-traumatic AC joint arthritis is even more prevalent due to the high incidence of injury to the joint. Arthritic symptoms have been demonstrated in Grade I and II sprains of the AC joint in 8% and 42% of patients, respectively.[1]
Diagnosis[edit | edit source]
Accurate diagnosis and localization of pathology to the AC joint is vital in determining the correct treatment protocol in order to avoid persistent shoulder pain. The proper diagnosis of ACJ arthritis requires a thorough history taking, physical exam, plain-film radiograph, and a diagnostic local anesthetic injection.[5]
History and on observation[edit | edit source]
- History of trauma: direct impact on the joint or a fall on an outstretched arm.
- Occupational history: an occupation that requires repeated overhead lifting activities, involvement in sports like weightlifting, rugby, etc. [2]
- A patient may complain of pain at night during sleeping on the affected shoulder.
- Patients may complain of popping, clicking, grinding, or catching sensation with the movement of their shoulder.[4]
- Possibly swelling in the shoulder as a presence of distal clavicle osteolysis.
On examination[edit | edit source]
- Patients often present with an intact range of motion with the exception of cross-body adduction, behind the back motions, and overhead reaching, which all produce pain localized to the AC joint.[1]
- Localized superior shoulder pain,[3]
- AC joint may be tender to palpation.
- Pain elicited to the deltoid area by the motion of forward flexion to 90° with horizontal adduction (cross-over test) or straight-ahead pushing (as in the bench press exercise).[1]
- The most sensitive tests for ACJ pain are acromioclavicular point tenderness and the Paxinos test.[2]
- Resisted AC joint extension test also helps to identify AC joint pathology.
- Acromioclavicular joint involvement can be confirmed by an injection of a local anesthetic. Injection of 0.5–2 mL of 1% or 2% lidocaine or 0.5 mL of 0.25 or 0.5% bupivacaine into the AC joint should provide a significant reduction in symptoms. A continuation of pain following anesthetic injection suggests other shoulder pathologies, most commonly rotator cuff injury.[1]
- Radiographic images:
- are the initial diagnostic imaging modality of choice, with anterior-posterior views demonstrating degenerative changes, subchondral cysts, sclerosis, osteophytes, and joint-space narrowing.
- The Zanca view, which consists of angling the X-ray source 10–15° superiorly and decreasing the kilovoltage to 50% standard exposure, is helpful in evaluating AC joint pathology by allowing visualization of distally projecting osteophytes of the acromion.
- Magnetic resonance imaging has the ability to detect capsular hypertrophy, effusions, and subchondral edema.[4][5]
Differential Diagnosis[edit | edit source]
Management[edit | edit source]
The management of ACJ pain appears to be determined by the degree of pain and disability.
Non- Surgical/ conservative[edit | edit source]
Non-operative management is usually considered first, with activity modification, physical therapy modalities, oral analgesics (NSAIDs), and injections of corticosteroid and local anesthetic all being options.
Local corticosteroid injection[edit | edit source]
Injections of 0.25–0.5 mL of betamethasone sodium phosphate and acetate or 0.25–0.5 mL methylprednisolone, 40 mg/mL are recommended. Limits of two to four injections per year with a total of twenty are recommended, as excessive corticosteroid administration may cause subcutaneous fat atrophy and dermal thinning. It is suggested that injections can provide good pain relief and be a helpful diagnostic test, but seem to be ineffective as a long term therapy.
Activity modification[edit | edit source]
It includes avoidance of repetitive motions causing the pain, such as push-ups, dips, flies, and bench press exercises.[1] Repetitive overhead activities, related sports need to be avoided until the health professionals recommend.
Physiotherapy treatment[edit | edit source]
Physiotherapy intervention should be individualized based on the grade of osteoarthritis, level of pain, and functional limitations.
Impairment based treatment:
- Pain management using electro-modalities, manual therapy
- Maintaining active ROM and strengthening scapular stabilizer muscles.
- Rotator cuff strengthening exercises.
- Postural correction: Pectoralis muscle stretching and retractors strengthening exercises.
Evidence
A prospective single-cohort study conducted by Harris et al. in 2012 regarding the effect of manual therapy in non-acute AC arthritis pain.
- It showed a statistically significant and clinically meaningful improvement in both functional and clinical outcome measures at 4 weeks and 6 months following manual therapy.
- The treatment duration was a 30-minute clinical sessions twice a week for 3 weeks.
- The primary treatment techniques were passive accessory glides of the distal end of the clavicle with the upper extremity in various physiological positions selected to make the ACJ treatment technique less painful. At other times, positions were selected to be more consistent with a position of pain during activity.
- After the 4-week follow-up visit, patients received instructions for a home-exercise program that consisted of strengthening and range-of-motion exercises.
- Statistically significant and clinically meaningful improvements were observed in all outcome measures at 4 weeks and 6 months, following a short series of manual therapy interventions. [3]
Surgical[edit | edit source]
Surgical treatment is only recommended if conservative treatment fails to provide adequate pain relief and persistent symptoms continue to interfere with activities of daily living after 6 months of intensive non-surgical treatment.
Distal clavicle excision (DCE)
- It is an operative approach also known as the “Mumford” procedure and is commonly performed.
- It was initially performed as an open procedure, first described in 1941 but now is performed arthroscopically.
- The procedure aims to produce a ‘gap’ between acromion and clavicle and involves resecting bone mainly from the distal end of the clavicle without compromising joint stability.[2]
- Open surgical complications for these procedures occur in 0% to 64% of cases and include infection, heterotopic ossification, joint instability, suprascapular neuropathy, and distal clavicle fracture, in addition to complications associated with anesthesia.[3] Other complications include weakness of the deltoid and trapezius muscles and clavicular instability.[1]
- Eskola et al investigated long-term results of patients managed with DCE for complaints of ACJ pain and reported that nearly 1 in 3 patients had poor long-term outcomes and advised against DCE for patients with higher functional demands on their shoulders.[3]
Future directions[edit | edit source]
A scoping review published in 2017
- reveals a lack of primary evidence regarding treatments and treatment pathways for ACJ pain. At no point have arthroscopic surgery, open surgery, steroid injections, and rehabilitation programs been compared directly.
- also shows making it difficult to delineate the cause of shoulder pain and the effectiveness of subsequent treatments as some bias was introduced by the fact that many patients with ACJ pathologies also had other concomitant shoulder pathologies, such as rotator cuff tears.[2]
Thus, proper assessment is necessary for the patient with shoulder pain followed by a holistic approach to treatment including lifestyle modification, education, medication, physiotherapy, and if necessary surgery followed by proper rehabilitation.
Related pages[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Docimo S, Kornitsky D, Futterman B, Elkowitz DE. Surgical treatment for acromioclavicular joint osteoarthritis: patient selection, surgical options, complications, and outcome. Current Reviews in Musculoskeletal Medicine. 2008 Jun 1;1(2):154-60.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Chaudhury S, Bavan L, Rupani N, Mouyis K, Kulkarni R, Rangan A, Rees J. Managing acromio-clavicular joint pain: a scoping review. Shoulder & Elbow. 2018 Jan;10(1):4-14.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Harris KD, Deyle GD, Gill NW, Howes RR. Manual physical therapy for injection-confirmed nonacute acromioclavicular joint pain. journal of orthopaedic & sports physical therapy. 2012 Feb;42(2):66-80.
- ↑ 4.0 4.1 4.2 Vaishya R, Damor V, Agarwal AK, Vijay V. Acromioclavicular arthritis: A review. Journal of arthroscopy and joint surgery. 2018 May 1;5(2):133-8.
- ↑ 5.0 5.1 Buttaci CJ, Stitik TP, Yonclas PP, Foye PM. Osteoarthritis of the acromioclavicular joint: a review of anatomy, biomechanics, diagnosis, and treatment. American journal of physical medicine & rehabilitation. 2004 Oct 1;83(10):791-7.
- ↑ AC Joint Pain Exercises for Shoulder Rehab. Available from: https://www.youtube.com/watch?v=m581lMvKSvw. [Lasted accessed: 2021/2/5]
- ↑ Mysportsdoc. Arthroscopic Distal Clavicle Excision. Available from: https://www.youtube.com/watch?v=OyvRDNJPC9Q. [Lasted Accessed: 2021/2/5]