Achilles tendon repair
Original Editor - Matt Anderson.
Top Contributors - Admin, Ben Kasehagen, Darine Mohieldeen, Rachael Lowe, Kim Jackson, Aminat Abolade, WikiSysop, Matt Anderson, Johnathan Fahrner, Tobias Meerts, Kai A. Sigel, 127.0.0.1, Tony Lowe and George Prudden
Description
[edit | edit source]
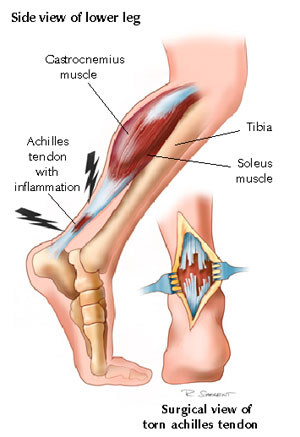
Achilles tendon rupture (ATR) is becoming more common, possibly due to an increase in the aging population and more middle aged people staying active in recreational activity.[1] Tendon degeneration with aging and certain medications (corticosteroids) could also be a predisposing risk for ATR. Achilles tendon repair is indicated when the Achilles tendon is ruptured, with the repair being performed within a week of the rupture, if possible. The common site of rupture is 2-6 cm from the calcaneal insertion . An ATR can occur from the following mechanisms: falling from a significant height, forceful plantar flexion of the ankle (as in jumping with an extended knee), or using the foot to break a fall if you stumble.
Indications[edit | edit source]
There is much disagreement in the literature about treatment for ATR with the two options comprising of a conservative or surgical approach. Some literature suggests that there is up to a 30% re-rupture rate for those who undergo conservative treatment, making the surgical option a good option. The argument for surgical repair also includes improved continuity of the tendon and possibly improved calf muscle function.
Clinical Presentation and Assessment[edit | edit source]
In 2010, the American Academy of Orthopaedic Surgeons published clinical guidelines regarding ATR.[2] They describe following a detailed history, a physical examination should include two or more of the following tests;
- Clinical Thompson test (Simmonds squeeze test) - The test is performed with the patient in prone. The tester gently squeezes the calf around the gastroc muscle bellies. The test is considered positive if there is little or no movement of the ankle into plantar flexion. The Sensitivity of this test is .96[3]
- Decreased ankle plantar flexion strength
- presence of a palpable gap (defect, loss of contour)
- Increased passive ankle dorsiflexion
Additional general clinical observations include: report of sharp onset of pain or the sound of a “gunshot” at the time of injury, and an inability to stand in plantarflexion. Immediately following the injury, the patient may complain of general pain, swelling and stiffness. This can be followed by bruising and a feeling of weakness
Pre-op[edit | edit source]
Prior to surgery general edema reduction should be used (Rest, Ice, Compression, Elevation). The surgery will ideally occur within one week of the rupture.
Surgery Description[edit | edit source]
File:Achilles tendon rupture 2.jpg
Many techniques exist for this surgery, including transverse, medial and longitudinal incisions. The ankle is placed in neutral position and the severed ends of the tendon are sutured together. The surgeon will then take the ankle through complete range of motion to look at the integrity of the repair. A cast is often applied, with the surgical technique determining how long the cast stays on.[4] Many surgeons are now focusing on early weight bearing and passive motion to improve tendon healing. A new minimally-invasive technique involves utilization of the peroneus brevis via two para-midline incisions. The technique reportedly preserves skin integrity over the site most prone to breakdown in a vertical incision, open reconstruction.[5] Another study recommended percutaneous repair in the recreational athlete and in patients concerned with cosmesis, and open repair for all high-caliber athletes who cannot afford any chance of rerupture."[6]
Post-op[4][edit | edit source]
Dutton describes three phases of post-surgical rehabilitation following Achilles tendon repair.
Phase I[edit | edit source]
Phase I typically lasts three weeks.
Goals of this phase are as follows:
- -Control edema and protect the repair site
- -Minimize scar adhesion and detrimental effects of immobilization
- -Progress to full weight bearing as tolerated/ indicated
- -Pain 5/10 or less, strength 4/5 all LE muscles except plantar flexors
Phase I interventions include:
- -Modalities for pain and edema
- -Stretching of large LE muscle groups, gastrocnemius/soleus added at week 3
- -AROM POD#2: plantar and dorsiflexion 3x5; 3 times daily; add inversion and
- eversion at week 2
- -Foot/ankle isometrics at week 2; band exercises week 3
- -Proprioceptive training for lower extremities; Gait training
- -Upper extremity cardiovascular exercise
- -Joint mobilization and soft tissue work, as indicated
Phase II[edit | edit source]
Phase II typically lasts from post op week 4-6.
Goals for this phase are as follows:
- -Normalized gait pattern
- -full ankle ROM
- -5/5 LE strength
- -Return to full ADL ability
- -Pain reported to be <2/10
- -Proprioceptive reactions equal to non-surgical side
Phase II interventions include:
- -Ankle flexibility at various knee angles
- -Progressive closed kinetic chain LE strengthening
- -Cardiovascular progression
- -Proprioceptive training on variety of surfaces
- -Manual resisted exercises and joint mobilization, as indicated
Phase III[edit | edit source]
Phase III typically lasts from post op week 6-15.
Goals for this phase are as follows:
- -Initiate running program
- -Improve balance and coordination
- -Increase velocity of activity
- -Return to sport
Phase III interventions include:
-Progressive ankle and LE strengthening
-Agility exercises
-Double heel raise/lower progressing to single leg heel raise at various speeds
Evidence Based Treatment Protocol[edit | edit source]
Week 0 - 2[edit | edit source]
Nil ankle RoM
Orthosis fixed at 30° of PF
Progress to full weight bearing (FWB)
Week 3 - 6[edit | edit source]
FWB
Active ankle RoM 0-30°
Orthosis limited to plantargrade (0° DF) to 30° PF
Week 7+[edit | edit source]
Full RoM
Nil orthosis
Key Evidence[edit | edit source]
Krueger-Franke M, Siebert CH, Scherzer S. Surgical treatment of ruptures of the Achilles tendon: a review of long-term results. Br J Sports Med. 1995;29(2):121-125.
Metzl JA, Ahmad CS, Levine WN. The ruptured Achilles tendon: operative and non-operative treatment options. Curr Rev Musculoskelet Med. 2008;1(2):161-164.
Ramelli FD. Diagnosis, management and post-surgical rehabilitation of an Achilles tendon rupture: a case report. J Can Chiropr Assoc. 2003;47(4):261-268.
Resources
[edit | edit source]
AAOS Guidlines for diagnosis and treatment of Acute Achilles Tendon Rupture
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1p5jL5WZFspdu6MqzF: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Chalmers J. Review Article: Treatment of Achilles Tendon Ruptures. J Ortho Surg. 2000;8(1):97-99.
- ↑ Chiodo CP, Glazebrook M, Bluman EM, Cohen BE, Femino JE, Giza E, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on treatment of Achilles tendon rupture. J Bone Joint Surg Am 2010;92(14):2466–8.
- ↑ Cleland J. Orthopaedic Clinical Examination: An Evidence Based Approach for Physical Therapists. Carlstadt, NJ: Icon Learning Systems:2005.
- ↑ 4.0 4.1 Dutton M. Orthopaedic Examination, Evaluation, and Intervention. New York, NY:McGraw-Hill:2004.
- ↑ Carmont MR, Maffulli N. Less invasive Achilles tendon reconstruction. BMC Musc Dis. 2007:8(100).
- ↑ Bradley JP, Tibone JE. Percutaneous and open surgical repairs of Achilles tendon ruptures: A comparative study. AJSM. 1990;18:188-195.
- ↑ Brumann, M., Baumbach, S. F., Mutschler, W., & Polzer, H. Accelerated rehabilitation following Achilles tendon repair after acute rupture-Development of an evidence-based treatment protocol. Injury. 2014