Achilles Tendon
Original Editor - Richard Benes
Top Contributors - Richard Benes, Kim Jackson, Joseph Ayotunde Aderonmu, Naomi O'Reilly, George Prudden, WikiSysop, Uchechukwu Chukwuemeka, Shrutika Das, 127.0.0.1, Admin, Laura Ritchie and Evan Thomas
Anatomy[edit | edit source]
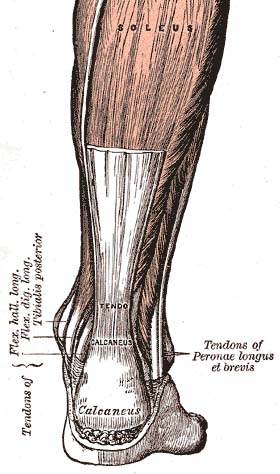
The Achilles (Calcaneal) tendon is a common tendon shared between the gastrocnemius and soleus muscles of the posterior leg. It connects the two muscle groups (collectively, triceps surae) to the calcaneus bone. Generally, the tendon winds 90 degrees on its path towards the heel, such that the gastrocnemius attaches laterally and the soleus attaches medially.[1]
A subcutaneous calcaneal bursa permits movement of the skin over the flexed tendon. A deep bursa of the Achilles tendon reduces friction to allow free movement of the tendon over the bone.[1]
Attachments[edit | edit source]
The tendon provides a distal attachment site for the gastrocnemius (lateral and medial heads) as well as the soleus muscles. It inserts onto the posterior surface of the calcaneus (heel bone). The plantaris tendon also fuses with the medial side of the Achilles tendon proximal to its attachment site.[2]
Function[edit | edit source]
Through the action of the triceps surae, which raises the heel and lowers the forefoot, the Achilles tendon is involved in plantar flexion of the foot (approximately 93% of the plantar flexion force).[1] The anatomy of the tendon provides for both elasticity (recoil) and shock-absorbance in the foot.[1] It is the largest and strongest tendon in the human body and is capable of supporting tensional forces produced by movement of the lower limb.[3]
Pathology/Injury[edit | edit source]
The Achilles tendon is susceptible to damage with repetitive use or overload. These types of injuries typically occur in athletes and are usually sports or exercise-related.[3]
The most common types of injuries are due to overuse and Achilles Tendon disorders, of which 55%-65% are diagnosed as Achilles Tendinopathy. Insertional issues (Retrocalcaneal Bursitis and Insertional Tendinopathy) account for 25%-35% of cases, with the remaining diagnosed as partial tears or undiagnosed complete ruptures.[3]
Complete Rupture of the Achilles Tendon has been estimated to occur at a rate of 5.5 to 9.9 per 100,000 in North America and between 6 to 18 per 100,000 in Europe.[4] Roughly 60-75% of ruptures take place in sporting activities, including basketball and soccer.[3]
Clinical Examination[edit | edit source]
Palpation[edit | edit source]
The foot is plantar flexed against resistance or gravity (body weight) while observing the posterior leg.
Examination[edit | edit source]
Achilles Tendinopathy[edit | edit source]
- Palpation and physical examination
- The VISA-A is a self-administered questionnaire that evaluates symptoms and their effect on physical activity for patients with chronic Achilles tendinopathy.
Achilles Rupture[edit | edit source]
- The Matles Test is a visual diagnostic test for suspected Achilles Tendon Rupture.
- The Thompson Test is used to identify the presence of a complete Achilles Tendon Rupture and is performed by squeezing the calf.
Physiotherapeutic Techniques[edit | edit source]
Achilles Tendinopathy[edit | edit source]
A summary of treatment interventions for Achilles Tendinopathy can be found in the Achilles Tendinopathy Toolkit.
Achilles Rupture[edit | edit source]
Optimal treatment of acute Achilles Rupture is a highly contested topic[8], but can be broken down into:
- Open Operative
- Percutaneous Operative
- Nonoperative Types.[3]
If a physician advocates for a non-surgical approach, the foot is typically placed in a cast or splint, such that it is held in plantar flexion. This treatment can be combined with early physiotherapy.[9]
More recently, evidence-based guidelines for managing Achilles Tendon Rupture have been released by the American Academy of Orthopaedic Surgeons (AAOS). None of the recommendations have a grading of "strong", but consensus recommendations based on expert opinion advocate the need for a detailed patient history and physical examination in diagnosis.[4][8] The group also recommends a more cautious approach in operative treatment for certain patients, including those with diabetes and/or neuropathy, aged 65 or older, who are obese or who have sedentary lifestyles, who are immuno-compromized, and who use tobacco.[4] The only recommendations rated as "moderate" in strength (fair quality evidence) were specifically for post-operative interventions. These were the suggestions for:
- Protective weight bearing and
- Use of a protective device that allows mobilization 2-4 weeks post-operatively.[8][4]
A review on the topic advocates for educating patients on the potential risks and benefits of each type of treatment, including operative and nonoperative types.[8]
Healing[edit | edit source]
A meta-analysis of randomized trials of Achilles tendon rupture repair has suggested that a nonoperative approach, in which plantar flexion is used to produce tendon apposition, can allow adequate healing. Functional bracing and modified postoperative mobilization, including daily active plantar flexion exercises, may stimulate tendon healing and reduce the potential rate of re-rupture.[9]
Resources[edit | edit source]
AAOS Guideline and Evidence Report: The Diagnosis and Treatment of Acute Achilles Tendon Rupture (2009)
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Moore KL, Agur AMR, Dalley AF. Essential clinical anatomy. 4th ed. Baltimore: Lippincott Williams & Wilkins, 2011.
- ↑ Drake RL, Vogl AW, Mitchell AWM. Gray's anatomy for students. 2nd ed. Philadelphia: Churchill Livingstone Elsevier, 2010.
- ↑ 3.0 3.1 3.2 3.3 3.4 Järvinen TA, Kannus P, Józsa L, Paavola M, Järvinen TL, Järvinen M. Achilles tendon injuries. Curr Opin Rheumatol 2001;13:150-5. http://journals.lww.com/co-rheumatology/Abstract/2001/03000/Achilles_tendon_injuries.9.aspx
- ↑ 4.0 4.1 4.2 4.3 American Academy of Orthopaedic Surgeons. The Diagnosis and Treatment of Acute Achilles Tendon Rupture. Rosemont: American Academy of Orthopaedic Surgeons, 2009. Available at: http://www.aaos.org/Research/guidelines/atrguideline.asp
- ↑ Clinically Relevant Technologi. Achilles Tendon Palpation Test (CR). Available from: https://www.youtube.com/watch?v=a9FI_0HpQ5Y [Accessed 18 Mar 2015]
- ↑ MSK Medicine. Matles Test. Available from: https://www.youtube.com/watch?v=7Vw9g-aI5pQ [Accessed 18 Mar 2015]
- ↑ Clinically Relevant Technologi. Thompson's Test (CR). Available from: https://www.youtube.com/watch?v=GtJF5cUmslI [Accessed 18 Mar 2015]
- ↑ 8.0 8.1 8.2 8.3 Pedowitz D, Kirwan G. Achilles tendon ruptures. Current Reviews in Musculoskeletal Medicine 2013;6(4):285-293. http://link.springer.com/article/10.1007%2Fs12178-013-9185-8 [Accessed 15 Mar 2015].
- ↑ 9.0 9.1 Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute achilles tendon rupture. J Bone Joint Surg Am 2012;94(23):2136-2143. http://jbjs.org/content/94/23/2136 [Accessed 30 Mar 2015].