Treacher Collins Syndrome
Definition[edit | edit source]
Treacher Collins syndrome (TCS) is a rare condition. Babies who have it are born with deformed ears, eyelids, cheekbones, and jawbones. There is no cure, but surgery can make a big difference. The condition is caused by an abnormal gene that affects how the face forms. Hearing loss is common.[1] Other names for this syndrome are mandibulofacial dysostosis, Treacher Collins-Franceschetti syndrome, Franceschetti-Zwahlen-Klein syndrome, and zygoauromandibular dysplasia.
- A child with TCS may have sleep apnea and/or conductive hearing loss ; the loss of ear function may require a resource to provide child hearing aids.
- Some individuals can be affected severely, and they may develop life-threatening breathing problems (infantile apnea).
- Other abnormalities may make breathing and feeding difficult for a child due to the narrowed obstruction of the nasal airways.
- A child may have features of “Pierre Robin sequence,” in which the tongue is located farther back in the throat than normal (glossoptosis), with or without an incomplete cleft palate of the mouth and airway obstruction.
Treacher Collins syndrome (TCS) affects approximately 1 in 50,000 live births.[1][2]
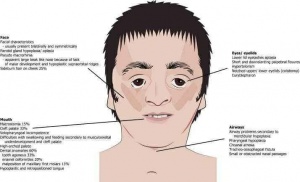
Signs & Symptoms[edit | edit source]
Signs and symptoms vary from almost unnoticeable face changes to severe facial and ear alterations, cleft palate and restricted airway. While some individuals may experience very mild symptoms, others have extremely severe symptoms that may have serious consequences, such as life-threatening airway problems.
Signs and symptoms of TCS include some parts of the body developing in abnormally or incompletely. These body areas include:
- Eyes, including lazy eye, an inability to focus, and vision loss
- Lower eyelids, which may include notching and sparse or absent eyelashes
- Cheekbones and jaw
- Chin
- Ears, which may include absent, small, malformed, or rotated ears
- Hair displacement, in which hair grows in front of the ears and to the lateral cheekbones
- An opening in the roof of the mouth called a cleft palate, with or without a cleft lip
- Airways
- Skull
- Nose
- Teeth
Hearing loss may occur due to abnormal development of the facial bones and incomplete or abnormal development of the ears. TCS may also cause a delay in motor and speech development. This condition can make it hard to breathe, sleep, eat, and hear. Problems with the teeth and dry eyes can lead to infections. Life can be hard for people with TCS. The deformities may lead to problems in family and social relationships.
Causes[edit | edit source]
TCS is caused by mutations in one of three genes:
- TCOF1[3]
- POLR1C
- POLR1D
A mutation in the TCOF1 gene causes the syndrome in 90–95 per cent of people with TCS.[1] A mutation in the POLR1C or POLR1D gene accounts for around 8 per cent of people with TCS.[4] All these genes play vital roles in the early development of facial bones and tissues. When they are mutated, certain cells involved in the development of bones and tissues of the face self-destruct. Approximately 40 per cent of people with TCS have a parent, or, rarely, two parents who carry affected genes.[5] In these cases, the gene abnormality causing TCS is inherited. The remaining 60 per cent of people develop TCS as the result of a new mutation — a mutation occurring for the first time. If the mutation has been detected within a family, there is an increased risk of a new baby getting it and having TCS. Therefore, a prenatal consultation is recommended in case of pregnancy.
Diagnosis[edit | edit source]
A diagnosis of TCS is made based on the following:
- Medical history
- Genetic testing- Genetic tests aim to detect mutations in the three genes that are known to cause TCS. Most of the time, genetic tests are not necessary to diagnose TCS, as a doctor can easily make a diagnosis by observing a person's symptoms. Genetic testing is helpful for further family planning.
- Physical and Radiographic examination- Radiographic examination may include different types of X-rays, or computed tomography (CT) scans to detect if the cheekbones and jawbone (mandible) have developed abnormally or incompletely way. A craniofacial CT scan can be performed to analyze the anatomy of the head, neck, ears, and ear canal. Doctors use this scan where there is hearing loss during the first 6 months of a child's life. An examination of the teeth, to look for dental abnormalities, can also be performed when teeth first appear.
After the initial diagnosis, other tests can help determine the severity of TCS. Doctors may examine the following:
- The airway to investigate predisposition to obstruction of the oropharynx
- The roof of the mouth for clefts
- The ability to swallow
- Hearing ability
- The eyes
Treatment[edit | edit source]
TCS can’t be cured. And no one treatment is best for everyone who has it. That’s because each case is different. It depends on the problems your child has or may have in the future. Care will usually involve several different health professionals, such as:
- A Paediatrician
- An Orthodontist
- A Dentist
- A Skull and Face Surgeon
- A Speech Therapist
- A Geneticist
- Nurses
- An Eye doctor
- A Hearing Specialist
- An Ear, Nose, and Throat Specialist.
For newborn infants with TCS, treatment will include procedures for improving breathing and how the airway works. Methods include special positioning of the infant and making an opening in the windpipe. Doctors can treat hearing loss caused by TCS with hearing aids, speech therapy, and integration into the education system. Surgeons can correct or rebuild the following areas if they are affected by abnormal or incomplete development:[6]
- The skull and face
- The roof of the mouth
- Cheekbones, jaw, and eye sockets
- The outer part of the ears
- Nose
- Teeth
- Lower eyelid
The age of the person will affect what surgery a doctor will recommend.[4] Repairs of the roof of the mouth are often carried out at 1–2 years of age. Cheek, jaw, and eye socket rebuilding is often done at 5–7 years of age. Ear corrections are usually made after 6 years of age. Jaw repositioning is typically done before 16 years of age. Other potential treatments are still under investigation, and no scientific results have yet been confirmed. They include:
- Adding stem cells to bone and cartilage to improve surgical outcomes when treating abnormalities of the skull and face.
- Treating TCS in the womb, when the embryo is still developing, by genetically manipulating a gene called p53 and blocking what it does.[7]
Genetic counselling may also be suggested for individual people with TCS or the whole family if the syndrome was inherited. At these meetings, people will learn about the outlook for a genetic disorder, and experts will advise them about what the chances are of passing the condition on.
Prognosis & Life expectancy[edit | edit source]
Usually, people with TCS grow to become functioning adults with normal intelligence. With proper management, life expectancy is approximately the same as in the general population. In some cases, the prognosis depends on the specific symptoms and severity of the affected person. For example, very severe cases of TCS can cause perinatal death because of a compromised airway.
Video[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 National Organization for rear disorders(NORD). Treacher collins syndrome. 2019. Available from: https://rarediseases.org/rare-diseases/treacher-collins-syndrome/
- ↑ Tse WK. Treacher Collins syndrome: New insights from animal models. Int J Biochem Cell Biol. 2016 Dec;81(Pt A):44-47.
- ↑ Van Gijn DR, Tucker AS, Cobourne MT. Craniofacial development: current concepts in the molecular basis of Treacher Collins syndrome. Br J Oral Maxillofac Surg. 2013;51(5):384-8.
- ↑ 4.0 4.1 Katsanis SH, Jabs EW. Treacher Collins Syndrome. GeneReviews 2004;1993-2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1532/
- ↑ Medline Plus.Treacher Collins syndrome. Available from: https://medlineplus.gov/genetics/condition/treacher-collins-syndrome/#inheritance (accessed 28 November 2017)
- ↑ Cobb AR, Green B, Gill D, Ayliffe P, Lloyd TW, Bulstrode N, Dunaway DJ. The surgical management of Treacher Collins syndrome. British Journal of Oral and Maxillofacial Surgery. 2014;52(7), 581–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24776174
- ↑ Jones NC, Lynn ML, Gaudenz K, et al. Prevention of the neurocristopathy Treacher Collins syndrome through inhibition of p53 function. Nat Med 2008;14(2):125-133.
- ↑ Ashley Davis. Treacher Collins Syndrome. Available from: http://www.youtube.com/watch?v=w5WC0bYsHM0 [last accessed 2019]