Ventilation and Weaning
Original Editor - The Open Physio Project
Top Contributors - Jagunath Selvanathan, Admin, Kim Jackson, Evan Thomas, Fasuba Ayobami, Mohit Chand, Rachael Lowe, Tony Lowe, WikiSysop, Karen Wilson, Vidya Acharya and Angeliki Chorti
Introduction[edit | edit source]
Ventilation can be defined as the process of exchange of air between the lungs and the ambient air.[1] In the clinical setting, a machine known as a mechanical ventilator is used to perform this function on patients faced with serious respiratory illness. Once a patient is stable and, in a position, to move towards spontaneous breathing it is important that that steps are taken to wean the patient of the dependency of supported breathing. Weaning is the gradual withdrawal of a patient from assisted breathing on a life-support system or other form of therapy.[1] Weaning a patient from a ventilator occurs when the condition of the patient improves, and a decision is made to remove them from the ventilator through a trial of spontaneous breathing through the endotracheal tube and eventually extubation (removal of the tube).
Goals of Mechanical Ventilation[edit | edit source]
The goals of mechanical ventilation are to:[2]
- Provide adequate (not perfect) oxygenation and ventilation
- Reduce our patient’s work of breathing
- Minimise the damage to the lung caused by the ventilator known as ventilator induced lung injury (VILI).
- Improve cardiac function
- Decreases preload
- Decreases afterload
- Decreases metabolic demand
Mechanical Ventilation[edit | edit source]
Mechanical ventilation can be: [2]
- Non - invasive (if patient can protect airway and is hemodynamically stable)
- Mask: usually orofacial to start
- Invasive
- Endotracheal tube (ETT)
- Tracheostomy – if upper airway is obstructed
Indications for Mechanical Ventilation[edit | edit source]
- Cardiac or respiratory arrest
- Tachypnea or bradypnea with respiratory fatigue or impending arrest
- Acute respiratory acidosis
- Refractory hypoxemia Refractory hypoxemia (when the P a O 2 could not be maintained above 60 mm Hg with inspired O 2 fraction (F I O 2 )>1.0)
- Inability to protect the airway associated with depressed levels of consciousness
- Shock associated with excessive respiratory work
- Inability to clear secretions with impaired gas exchange or excessive respiratory work
- Newly diagnosed neuromuscular disease with a vital capacity <10 capacity <10 - 15 mL/kg
- Short term adjunct in management of acutely increased intracranial pressure (ICP) [1][3]
Basic settings on a mechanical ventilator include:
- Mode
- Tidal Volume
- Respiratory rate (RR)
- Inspired oxygen concentration (Fio2)
- Positive end expiratory pressure (PEEP)
Mechanical ventilator breaths [2]
Breaths can be either controlled, assisted or supported by the ventilator.
- Controlled Breaths: These breaths are completely “controlled” by the ventilator. A ventilator is purposely never set up in a mode with controlled breaths only. However, controlled breaths are delivered for safety at a set time interval if your patient is paralyzed or doesn’t have a respiratory drive (sedation, comatose, etc.).
- Assisted Breaths: Unlike the controlled breaths, which come at a set time interval, assist breaths will be delivered to your patient if they attempt to trigger a breath. If your patient attempts a breath, then the ventilator will sense this, and deliver a full mechanical breath. For an assist breath, the patient must trigger the ventilator (sucking in on ETT and generate a change in pressure or flow), then the ventilator completely takes over and delivers a full breath
- Supported (Spontaneous) Breaths: These types of breaths are triggered by patient effort (like assisted breaths), but once triggered the ventilator will give you some support, but not full support like an assisted breath.
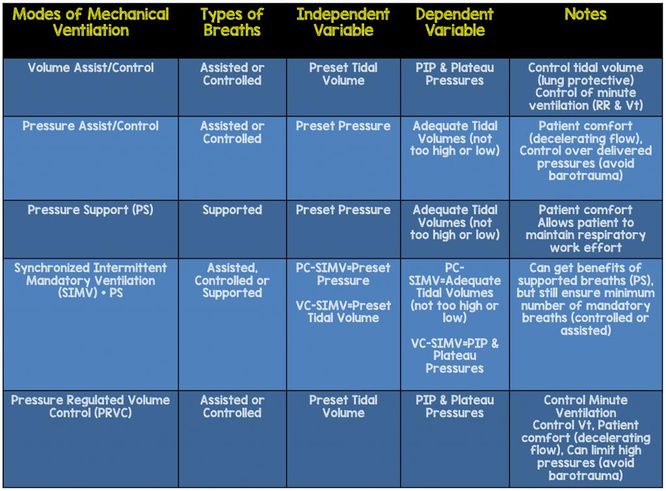
Modes of Mechanical Ventilation[edit | edit source]
The different modes of mechanical ventilators and all of them have different roles. See below for some examples: [2]
- Volume assist/control
- Pressure assist/control
- Pressure support (PS)
- Synchronised intermittent mandatory ventilation (SIMV) +PS
- Pressure regulated volume control (PRVC)
Procedure of Weaning patient[edit | edit source]
Weaning is gradual reduction of ventilation. A new systematic review suggests that noninvasive ventilation after early extubation helps in reducing the total days spent on invasive mechanical ventilation; also, the patients spending less time on invasive ventilation had lower rates of ventilator-associated-pneumonia. [4] In some cases, this process is rapid and uneventful; however, for some patients the process may be prolonged for days or weeks. Weaning is a term that is used in two separate ways. Firstly, it implies the termination of mechanical ventilation and secondly the removal of any artificial airway. [5]
When to wean[5][edit | edit source]
- Normalised I:E ratio
- Reducing FiO2 (usually <0.5)
- No requirement for high PEEP
- Appropriate underlying respiratory rate
- Appropriate tidal volume with moderate airway pressures
The procedure is as follows:
- Explanation of the procedure to the patient, assuring them it is only for a trial period
- The ventilator support is gradually reduced (e.g. reducing pressure during pressure support)
- The patient is placed into a better postural position (e.g. sitting upright or half-sitting)
- The airway is suctioned
- The patient is disconnected from the ventilator and given oxygen or mechanical assistance (CPAP)
- The patient is encouraged to breathe spontaneously
- The patient is monitored for signs of laboured breathing, anxiety or an increase in PaCO2
- Extubation should occur as soon as possible because breathing through an endotracheal tube increases the work of breathing
- Encourage the patient to cough after being extubated
Patients may be extubated when they are alert, show a stable breathing pattern and control their airway. Difficulties in weaning patients from a ventilator can occur due to:
- Inspiratory muscle atrophy
- Fatigue
- Paralysis of the diaphragm
- A fear of suffocating
Physiotherapy Role in Mechanical Ventilation and Weaning[edit | edit source]
Traditionally, physiotherapists have been involved in the respiratory care of patients on mechanical ventilation in ICU.[3] The respiratory care involves optimisation of ventilation, airway clearance, prevention of pulmonary complications, and hastening weaning from mechanical ventilation.
Techniques used by physiotherapy to help improve patient breathing and wean patients off ventilators may include:
- Suctioning
- Postural drainage
- Central lavage (Paediatrics)
- Percussion
- Vibrations
Guidelines[edit | edit source]
1) Evidence-Based Practice of Weaning from Ventilator: A Review[6]
2) Clinical Practice Guideline: Liberation from Mechanical Ventilation in Critically Ill Adults[7]
3) Ventilator Discontinuation Protocols[8]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Miller-Keane OT, O’Toole M. Miller-Keane encyclopedia and dictionary of medicine, nursing and allied health.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 MD, F. (2019). Simplifying Mechanical Ventilation – Part I: Types of Breaths - REBEL EM - Emergency Medicine Blog. [online] REBEL EM - Emergency Medicine Blog. Available at: http://rebelem.com/simplifying-mechanical-ventilation-part/ [Accessed 2 Mar. 2019].
- ↑ 3.0 3.1 Bhat A, Vasanthan LT, Babu AS. Role of physiotherapy in weaning of patients from mechanical ventilation in the Intensive Care Unit. Indian Journal of Respiratory Care. 2017 Feb 1;6(2):813.
- ↑ Vaschetto, R., Pecere, A., Perkins, G.D., Mistry, D., Cammarota, G., Longhini, F., Ferrer, M., Pletsch-Assunção, R., Carron, M., Moretto, F. and Qiu, H., 2021. Effects of early extubation followed by noninvasive ventilation versus standard extubation on the duration of invasive mechanical ventilation in hypoxemic non-hypercapnic patients: a systematic review and individual patient data meta-analysis of randomized controlled trials. Critical Care, 25(1), pp.1-11.
- ↑ 5.0 5.1 Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, Pearl R, Silverman H, Stanchina M, Vieillard-Baron A, Welte T. Weaning from mechanical ventilation. European Respiratory Journal. 2007 May 1;29(5):1033-56.
- ↑ Sengupta S, Chakravarty C, Rudra A. Evidence-Based Practice of Weaning from Ventilator: A Review.
- ↑ Gregory A Schmidt, Timothy D Girard, John P Kress, Peter E Morris, Daniel R Ouellette, Waleed Alhazzani, Suzanne M Burns, Scott K Epstein, Andres Esteban, Eddy Fan, Miguel Ferrer, Gilles L Fraser, Michelle Ng Gong, Catherine L Hough, Sangeeta Mehta, Rahul Nanchal, Sheena Patel, Amy J Pawlik, William D Schweickert, Curtis N Sessler, Thomas Strøm, Kevin C Wilson, Jonathon D Truwit; ATS/CHEST Ad Hoc Committee on Liberation from Mechanical Ventilation in Adults Official Executive Summary of an American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from Mechanical Ventilation in Critically Ill Adults, Assessed on 13/4/2023.
- ↑ Haas CF, Loik PS. Ventilator discontinuation protocols. Respiratory care. 2012 Oct 1;57(10):1649-62.