Peptic Ulcers
Original Editors -Emily Hays from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Hays, Admin, WikiSysop, Wendy Walker, Evan Thomas, Kim Jackson and Lucinda hampton
Description
[edit | edit source]
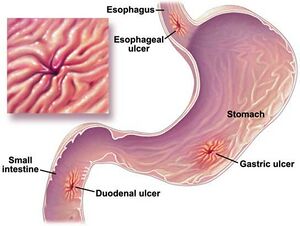
Peptic ulcers are the result of deterioration of the mucosal lining of the stomach and duodenum that can lead to damage of the gastrointestinal tissue. Pepsin, a catalytic enzyme that assists in protein breakdown, increases the gastric acidity in the stomach and assists in digestion. This production of excessive acid can overwhelm the protective lining of mucus within the stomach and duodenum. The stomach tissue cannot handle the acidity and begins to erode.[1]
There are three classifications of Peptic Ulcers:
- Stomach
- Duodenal
- Stress
Prevalence/Incidence[edit | edit source]
According to the National Institute of Health, one in 10 Americans will suffer an ulcer. Over 500 million people are newly diagnosed each year while 4 million cases reported are recurrent. Although ulcers can occur at any age, including infancy, stomach ulcers are more common after 60 years of age and are typically seen more in women than men. Duodenal ulcers are more commonly seen during the third and fifth decades and effect men more than women. Stress Ulcers have not been identified to be more prominent at any age, but rather more apparent in high stress living environments and those individuals who have suffered from a trauma such as a burn or gastrointestinal surgery. You are twice as likely to suffer from a peptic ulcer if you are African American or Hispanic.[2][3]
Causes[edit | edit source]
Ulcerations can occur due to a bacterial infection of the mucosal lining of the stomach. Helicobacter pylori more commonly known as H. Pylori, causes an overproduction of stomach acid which can overpower the membranes and cause a breakdown of the stomach lining.
H.Pylori is a recently discovered bacteria that has been recognized to flourish in the acidic environment of the stomach and duodenum. Researchers have identified that this bacteria could be transmitted orally by way of residual fecal matter in food or water. For more information please visit The Helicobacter Foundation.[4]
Peptic ulcers can occur also with prolonged NSAIDs use, hiatal hernia, vitamin deficiency such as folic acid and vitamin C can also cause an imbalance of gastric juices which can make the stomach susceptible to erosion. Other research suggests that ulcers are a side effect psychological stress and are more prominent in individuals with poor coping skills. [5]
Characteristics[edit | edit source]
Three stages of ulceration have been identified:
- Erosion is the first stage where a marked destruction of the mucosal lining approximately 1-2 cm across.
- Stage two, considered a True Ulcer can emerge if erosion is not care for and can be identified by the marked or scarred disruption of the smooth tissue in the stomach and duodenum.
- The final and most life threatening stage is a Bleeding Ulcer. This type of ulcer is a partial or complete hole in the stomach tissue causing hemorrhage. This condition is a medical emergency and can cause significant GI complications. [1][3]
Risk Factors [edit | edit source]
- Are over the age of 50.
- Consume large quantities of alcohol of a regular basis.
- Smoke cigarettes or use tobacco.
- Have a family history of ulcer disease.
You’re at risk for NSAID-induced ulcers if you:
- Had previous occurence of ulceration or gastrointestinal bleeding.
- Are using steroid medication or on a blood thinner.
- Consume alcohol or use tobacco on a regular basis.
- Have a high sensitivity to medications, experiencing an upset stomach or heartburn.
- Take several different medications that contain aspirin and other NSAIDs.[6]
Clinical Presentation[edit | edit source]
Symptoms can easily be dismissed during a physical therapy evaluation if not directly asked to the patient since some symptoms may feel unrelated to the patient. A patient may present with low back pain that they cannot identify specifically to an event or particular injury. When prompted, the patient may be able to assess their pain characteristics as a dull or gnawing ache that can occur usually 1-3 hrs after eating. [5][6]The pain can be intermittent but usually consistent for a period of time until digestion is complete. Patients may report that pain can be alleviated with eating a small amount of food or taking an antacid, but will return after a full meal. Severe ulceration can cause a blockage and does not allow food to move from the stomach to the duodenum. This typically causes significant pain, nausea and vomiting.
Additional Symptoms include:
- Night pain from laying flat
- GERD
- Weight loss
- Bloating/distended stomach
- Burping
- Feeling of fullness/poor appetite
- Melena
- Coffee-ground vomitus
- Light-headedness
- Right shoulder pain that changes in the position cannot alter
Although patient education and referral is an important aspect for the physical therapist management; peptic ulcers should be managed by a licensed medical professional such as a general practitioner or gastroenterologist.
Diagnostic Tests/Lab Values[edit | edit source]
- Upper GI: Series of x-rays of the GI tract including the esophagus, stomach and duodenum. The patient will need to ingest a barium solution which allows these structures to be viewed by a radiologist with more clarity.
- Endoscopy: this is a procedure using a thin tube connected to a lit camera which is inserted through the mouth into esophagus and allows a physician to see an ulcer and determine its severity.
- Blood tests can also be performed to determine if a patient has the H. pylori bacterial infection.
Medications/Medical Management[edit | edit source]
Once the source of ulceration has been determine various drugs are available for the physician to use based on the patients presentation.
If H. pylori is determined to be the cause:
- Clarithromycin
- Tetracycline
- Amoxicillin
- Metronidazole
- Bismuth (the main ingredient in Pepto-Bismol)
Proton pump inhibitors like omeprazole (Prilosec), lansoprazole (Prevacid), or esomeprazole (Nexium) have shown effectiveness with H. pylori but can also be used for non-bacterial treatment of ulcers.
Other medications that may be used for ulcer symptoms or disease are:
Excessive NSAIDs use has been linked to the destruction of the stomach lining which can cause an ulcer to occur. Some patients may be required to use NSAIDs for other health conditions and may be medications, such as misoprostol or sucralfate (protect the mucosal lining of the stomach and duodenum).
Medical Management includes evaluation of external factors contributing to the ulceration. Revision of medications, diet, cessation of smoking and alcohol use. Additionally, surgical procedures may be warranted if healing of ulcer cannot be done conservatively.[7][8]
Surgical management includes:
- Antrectomy: Removal of the lower third of the stomach
- Hemigastrectomy: Removal of the lower half of the stomach
Differential Diagnosis[edit | edit source]
Physical Therapist's must recognize the potential for gastrointestinal problems during an exam due to the occurrence of ulcers mimicking musculoskeletal problems. Low back pain with an insidious onset has been identified as one of the more common complaints. Thoracic pain, in particular T6-T10 has been identified as a referral pain site.
Additionally, other conditions can be associated with the clinical presentation. These include:
- GERD
- Diverticulitis
- Pancreatitis
- Pancreatic Carcinoma
- Ulcerative Colitis
- Crohn's Disease
- Irritable Bowel Syndrome
- Colorectal Cancer
Referral to a physician should be warranted for any of the above mention as well as peptic ulcers if:
- The patient indicates that symptoms increase with a few hours of taking NSAIDs
- GI symptoms presented within the same time frame as the musculoskeletal complaints
- Pain in the shoulder, back or sacral area that are alleviated after meals or bowel movements.
- Positive McBurney's or pain produced with heel tap.
- Joint pain with recognizable development of rosacea
- Increase in muscle guarding and pain during therapeutic intervention over the course of several treatments. [5]
Case Studies[edit | edit source]
- Peptic Ulcer Disease in a General Adult Population
- Effects of Helicobacter pylori and Nonsteroidal Anti-Inflammatory Drugs on Peptic Ulcer Disease: A Systematic Review
Resources[edit | edit source]
- American Gastroenterologist Association
- Incidence and Risk Factors for Self-reported Peptic Ulcer Disease in the United States
- Prevalence and incidence of peptic ulcer disease in a Danish County a prospective cohort study
- Peptic ulcer disease today
- Management of Complicated Peptic Ulcer Disease
References[edit | edit source]
- ↑ 1.0 1.1 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis, Missouri; Saunders Elsevier: 2009. p842-45
- ↑ U.S. National Library of Medicine, National Institute of Health. Medline Plus: Peptic Ulcer. http://www.nlm.nih.gov/medlineplus/ency/article/000206.htm (accessed 15 March 2010).
- ↑ 3.0 3.1 National Institute of Diabetes and Digestive and Kidney Diseases. National Digestive Diseases Information Clearinghouse. http://digestive.niddk.nih.gov/ddiseases/pubs/hpylori/ (accessed 1 March 2010).
- ↑ http://www.helico.com/
- ↑ 5.0 5.1 5.2 Goodman CC, Snyder TK. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th ed. St. Louis, Missouri: Saunders Elsevier; 2007. P366-408.
- ↑ 6.0 6.1 American Gastroenterological Association Patient Center. Disease fact sheet: Peptic Ulcer Disease. http://www.gastro.org/wmspage.cfm?parm1=478 (accessed 15 March 2010)
- ↑ National Institute of Health. DailyMed: Medications. http://dailymed.nlm.nih.gov/dailymed/about.cfm (acessed 30 March 2010).
- ↑ Gladson B. Pharmacology for Physical Therapists. St Louis, MO 63146, Elsevier: 2006