Inguinal Hernia
Original Editors - Lindsey Roederer and Stephanie McCauley from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Admin, Lindsey Roederer, Stephanie McCauley, Lucinda hampton, Elaine Lonnemann, WikiSysop, Kim Jackson and Wendy Walker
Introduction[edit | edit source]
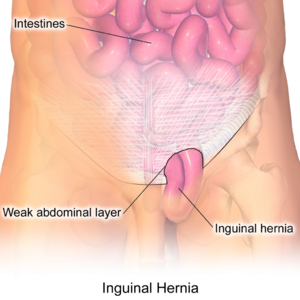
Inguinal hernias (IH) are groin herniation that occurs above the inguinal ligament and through the inguinal canal. They are a subset of abdominal wall hernias.[1]
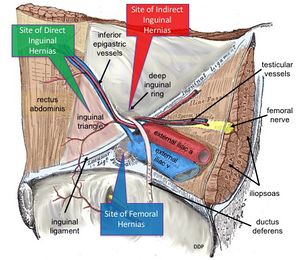
Classification: broadly divided into two types:
- Direct hernia: occurs when a portion of the intestine protrudes directly outward through a weak point in the abdominal wall eg may be caused by a deficiency in the number of transversus abdominus aponeurotic fibers.
- Indirect hernia: occurs when a portion of the intestine pushes downward through the deep inguinal ring into the inguinal canal where the testes descend into the scrotum before birth (males) or to the labia (females) [2]
Epidemiolgy[edit | edit source]
Abdominal wall hernias are common, with a prevalence of 1.7% for all ages and 4% for those aged over 45 years. Inguinal hernias account for 75% of abdominal wall hernias, lifetime risk of 27% in men and 3% in women.[3] They are most often acquired.[1]
Little is known about the epidemiology of inguinal hernia, a common easily treatable surgical condition, in resource-poor settings.[4]
Etiology[edit | edit source]
Increased risk for
- Indirect inguinal hernia include: Prematurity and low birth weight; urologic conditions; abdominal wall defects; family history
- Direct inguinal hernia, is a consequence of weakened abdominal musculature, often brought on by: Advanced age; strain; previous abdominal surgery
Direct hernias, in particular, are rare in women since the broad ligament (uterine ligament) acts as an additional barrier.[1]
Characteristics/Clinical Presentation[edit | edit source]
An inguinal hernia can present with the following signs and symptoms:
- Intermittent or persistent bulge in the groin [2]
- Pain or discomfort in the groin, especially when lifting, coughing, or bending[5]
- Weakness or pressure in the groin[5]
- Men can experience pain and swelling in the scrotum[5]
Inguinal hernias tend to be more noticeable following a heavy meal or after standing for a prolonged period of time. The pain associated with an inguinal hernia is usually sharp and localized. It can be heightened by changes in position, physical exertion, and with any activity causing the Valsalva maneuver.[2]
Differential Diagnosis [edit | edit source]
Possible imaging differential considerations include
- femoral hernia: often remain lateral to the pubic tubercle and compress the femoral vein
- hydrocele (may coexist)
- varicocele[1]
Medications[edit | edit source]
Antibiotics are prescribed for strangulated hernias if ischemic bowel or infection is suspected. Over-the counter or prescribed medication for pain relief is utilized following surgical procedures[6].
Surgery[edit | edit source]
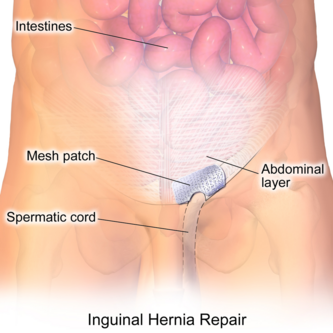
Surgical treatment options include
- Herniorrhaphy (Open hernia repair) - Local or general anesthesia is administered. The surgeon makes an incision in the groin, moves the hernia back into the abdomen, and reinforces the muscle wall with stitches.
- Hernioplasty - The area of muscle weakness is reinforced with a synthetic mesh or screen to provide additional support. This method may be utilized in open or laparoscopic repairs.
Medication is prescribed for pain management following surgery. Vigorous activity and heavy lifting are restricted for several weeks[6].
Conservative Management[edit | edit source]
Generally inguinal hernias should be repaired. M Hammoud and J Gerken (2018)[7] state this has been brought into question in recent reports. Possibly watchful waiting is a safe and acceptable option for those with who are asymptomatic or minimally symptomatic. The as the risk of incarceration and strangulation recent studies was minimal.[7]
Physical Therapy Management[edit | edit source]
Education - Physical therapists educate clients on work strategies, including body mechanics, proper breathing, and lifting techniques. By reducing strain and increased intraabdominal pressure, one may decrease the risk of developing a hernia or worsening an already existing hernia[2].
Screening - Obtaining a thorough medical history and conducting a physical examination is critical in determining the need for potential referral to a physician for diagnosis of an inguinal hernia. To palpate for an inguinal hernia, place hand at the location of the inguinal canal, superior to inguinal ligament and just lateral to the scrotum. Have the patient strain down or cough in standing to feel for a palpable mass [8].
Postoperative Rehabilitation - Often, patients are not seen for post-operative rehabilitation of an inguinal hernia repair. However, patients may require physical therapy services in order to return to prior level of function. A rehabilitation program will include posture exercises, education of proper body mechanics, and core strengthening. The program will be progressed as appropriate to include sport or work-specific functional activities[2].
See also Assessment of Fitness for Return to Work
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Radiopedia Inguinal Hernia Available: https://radiopaedia.org/articles/inguinal-hernia(accessed 20.12.2022)
- ↑ 2.0 2.1 2.2 2.3 2.4 Goodman CC, Fuller KS, Pathology: Implications for the Physical Therapist. The Gastrointestinal System. Saunders, Elsevier Inc., 2009. p870-74.
- ↑ Jenkins JT, O’dwyer PJ. Inguinal hernias. Bmj. 2008 Jan 31;336(7638):269-72.Available;https://www.bmj.com/content/336/7638/269 (accessed 20.12 2022)
- ↑ Beard JH, Oresanya LB, Ohene-Yeboah M, Dicker RA, Harris HW. Characterizing the global burden of surgical disease: a method to estimate inguinal hernia epidemiology in Ghana. World journal of surgery. 2013 Mar;37(3):498-503. Available:https://pubmed.ncbi.nlm.nih.gov/23224074/ (accessed 20.12.2022)
- ↑ 5.0 5.1 5.2 Mayo Clinic. Inguinal Hernia. http://www.mayoclinic.com/health/inguinal-hernia/DS00364/DSECTION=symptoms (accessed 10 February 2013)
- ↑ 6.0 6.1 U.S. National Library of Medicine. Inguinal Hernia- discharge. http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000274.htm (accessed 2 Feb 2013)
- ↑ 7.0 7.1 Hammoud M, Gerken J. Inguinal hernia.Available:https://www.ncbi.nlm.nih.gov/books/NBK513332/ (accessed 20.12.2022)
- ↑ Moore KL, et al, Essential Clinical Anatomy. Abdomen. Lippincott, Williams, and Wilkins, 2011. p134-5.