Proximal Hamstring Tendinopathy: Difference between revisions
Kai A. Sigel (talk | contribs) (Added a video for the bent knee stretch test) |
Evan Thomas (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor ''' - [[User:Melissa De Maeyer|Melissa De Maeyer]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
= | |||
= Description = | |||
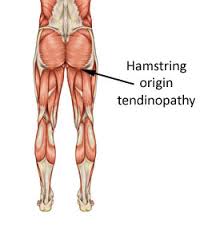
Hamstring origin tendinopathy, also called proximal hamstring tendinopathy or high hamstring tendinopathy, are a group of pathologies of the proximal hamstring tendon. They contain tendon degeneration, partial tearing and peritendinous inflammatory reaction.<ref name="5">Maurice H. Zissen, et al. High Hamstring Tendinopathy: MRI and Ultrasound Imaging and Therapeutic Efficacy of Percutaneous Coorticosteroid Injection [Internet]. American Roentgen Ray Society 2010.Available from: http://www.ajronline.org/doi/pdf/10.2214/AJR.09.3674
Level of evidence 2B, grades of recommendation B</ref> | Hamstring origin tendinopathy, also called proximal hamstring tendinopathy or high hamstring tendinopathy, are a group of pathologies of the proximal hamstring tendon. They contain tendon degeneration, partial tearing and peritendinous inflammatory reaction.<ref name="5">Maurice H. Zissen, et al. High Hamstring Tendinopathy: MRI and Ultrasound Imaging and Therapeutic Efficacy of Percutaneous Coorticosteroid Injection [Internet]. American Roentgen Ray Society 2010.Available from: http://www.ajronline.org/doi/pdf/10.2214/AJR.09.3674
Level of evidence 2B, grades of recommendation B</ref> | ||
| Line 10: | Line 11: | ||
[[Image:Hamstring origin tendinopathy.jpg|center]] | [[Image:Hamstring origin tendinopathy.jpg|center]] | ||
= | = Clinically Relevant Anatomy = | ||
One of the most important muscle groups in running is the hamstring. They are active at multiple points in the gait cycle, namely the knee flexion and the hip extension. | One of the most important muscle groups in running is the hamstring. They are active at multiple points in the gait cycle, namely the knee flexion and the hip extension. | ||
The distal attachment is located on the top of your tibia, just behind the knee. The origin is divided in three branches, one starting from the femur and the two remaining ones starting from the ischial tuberosity. The junction between the tendons of the hamstrings and the ischial tuberosity is the area affected by high hamstring tendinopathy. The tendon’s thickness, fibrousness and poor blood supply is the cause of a difficult healing.<ref name="10">High hamstring tendinopathy injuries – Signs, symptoms and research-backed treatment solutions for a literal pain in the butt.
Available from:
http://runnersconnect.net/running-injury-prevention/high-hamstring-tendinopathy-injuries-a-pain-in-the-butt/</ref> | The distal attachment is located on the top of your tibia, just behind the knee. The origin is divided in three branches, one starting from the femur and the two remaining ones starting from the ischial tuberosity. The junction between the tendons of the hamstrings and the ischial tuberosity is the area affected by high hamstring tendinopathy. The tendon’s thickness, fibrousness and poor blood supply is the cause of a difficult healing.<ref name="10">High hamstring tendinopathy injuries – Signs, symptoms and research-backed treatment solutions for a literal pain in the butt.
Available from:
http://runnersconnect.net/running-injury-prevention/high-hamstring-tendinopathy-injuries-a-pain-in-the-butt/</ref> | ||
[[Image:Hamstring tendons.png]]<br>The muscles of the hamstrings have a higher proportion of type 2 muscle fibers than the other muscles of the lower extremity. This suggests that these muscles can generate high intrinsic tension force. While running, the time increases that the hamstrings are under maximal stretch. The hamstrings and their tendon attachments have to endure heavy charges or high tensions because of these two forces, namely during eccentric contractions.<ref name="4">Michael Fredericson, et al. High Hamstring Tendinopathy in Runners. Meeting the Challenges of Diagnosis, Treatment, and Rehabilitation [Internet]. The Physician and Sportsmedicine 2005. Available from: http://www.agilept.com/downloads/high-hamstring-tendinopathy-in-runners.pdf - | [[Image:Hamstring tendons.png]]<br>The muscles of the hamstrings have a higher proportion of type 2 muscle fibers than the other muscles of the lower extremity. This suggests that these muscles can generate high intrinsic tension force. While running, the time increases that the hamstrings are under maximal stretch. The hamstrings and their tendon attachments have to endure heavy charges or high tensions because of these two forces, namely during eccentric contractions.<ref name="4">Michael Fredericson, et al. High Hamstring Tendinopathy in Runners. Meeting the Challenges of Diagnosis, Treatment, and Rehabilitation [Internet]. The Physician and Sportsmedicine 2005. Available from: http://www.agilept.com/downloads/high-hamstring-tendinopathy-in-runners.pdf - Level of evidence 2A, grades of recommendation B</ref> | ||
(For extra information about pathology mechanisms see [http://www.physio-pedia.com/Tendinopathy Tendinopathy]) | (For extra information about pathology mechanisms see [http://www.physio-pedia.com/Tendinopathy Tendinopathy])<br> | ||
= Epidemiology / Etiology = | = Epidemiology / Etiology = | ||
| Line 24: | Line 25: | ||
Hamstring origin tendinopathy may arise after an acute tear at the origin that is not adequately treated. Still in most cases it’s a common overuse injury that is often seen in runners (more in middle- or long-distance runners than sprinters). It typically occurs with repetitive jumping, kicking and running activities. The hamstrings are prone to this type of injury as they contribute to the decelerating of the extension of the knee during activities such as sprinting and hill climbing. (Petersen J. et al, 2005) | Hamstring origin tendinopathy may arise after an acute tear at the origin that is not adequately treated. Still in most cases it’s a common overuse injury that is often seen in runners (more in middle- or long-distance runners than sprinters). It typically occurs with repetitive jumping, kicking and running activities. The hamstrings are prone to this type of injury as they contribute to the decelerating of the extension of the knee during activities such as sprinting and hill climbing. (Petersen J. et al, 2005) | ||
The following factors can also increase the risk of hamstring origin tendinopathy: <br>'''Intrinsic factors:''' | |||
*Malalignments | *Malalignments | ||
*Leg length discrepancy | *Leg length discrepancy | ||
| Line 31: | Line 31: | ||
*Decreased flexibility | *Decreased flexibility | ||
A study of stretching found that there are more hamstring problems with persons who didn’t stretch before participating in sports.<ref name="16">P.BRUKNER &amp;amp;amp;amp;amp;amp;amp;amp; K. KAHN, clinical sports medicine, McGraw-Hill, Australia, 2005 (third edition), P388-390</ref> | |||
*Joint laxity | *Joint laxity | ||
*Female gender | *Female gender | ||
*Age - When you get older, there is a reduction in muscle fiber size and number. This leads to a loss of mass and strength.<ref name="16" /> | *Age - When you get older, there is a reduction in muscle fiber size and number. This leads to a loss of mass and strength.<ref name="16" /> | ||
*Overweight | *Overweight | ||
*Proprioceptive weakness<ref name="kristen">White, K. E., High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine 2011, 10 (2), 93-99
Level of evidence 4. grades of recommendation C</ref> | *Proprioceptive weakness<ref name="kristen">White, K. E., High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine 2011, 10 (2), 93-99
Level of evidence 4. grades of recommendation C</ref> | ||
*Ischial tuberosity tenderness | *Ischial tuberosity tenderness | ||
*Core weakness | *Core weakness | ||
| Line 53: | Line 53: | ||
*environmental malconditions | *environmental malconditions | ||
*poor equipment | *poor equipment | ||
*Insufficient warming up - | *Insufficient warming up - A warm-up with isometric contractions increases strength and length of the muscle.<ref name="16" /> | ||
*Excessive training | *Excessive training | ||
*Fatigue - | *Fatigue - The muscle has less energy. There is also a lack of concentration, coordination and technique.<ref name="16" /> | ||
<br> | <br> | ||
Apparently core weakness and pelvic dysfunction seem to be closely related to the development of a hamstring tendinopathy.<ref name="fred" /> | Apparently core weakness and pelvic dysfunction seem to be closely related to the development of a hamstring tendinopathy.<ref name="fred" /> The tendinopathy usually starts with micro-damage without a remarkable trauma. Normally the tendon is capable to intrinsic repair, meaning that the consequences of this injury are little. Sometimes, imbalance can cause further damage and failed healing. All of this leads to the formation of tendinosis. (Kannus 1997, Sharma and Maffulli 2005, Warden 2007.) Intrinsic and extrinsic factors contribute to the formation of this injury.<ref name="10" /><br> | ||
= <br>Characteristics / Symptoms = | = <br>Characteristics / Symptoms = | ||
| Line 109: | Line 109: | ||
The pain increases while repetitive activity (such as long-distance running) and in worse cases pain is also mentioned while the person is sitting or driving a car. Usually there’s no acute trauma when the pain starts to appear, it gradually gets worse<ref name="13">Puranen J.; Orava S., The hamstring syndrome. A new diagnosis of gluteal sciatic pain, American Journal of Sports Medicine, 1988, 16(5): 517 – 521.
Level of evidence 4, grades of recommendation C</ref>. | The pain increases while repetitive activity (such as long-distance running) and in worse cases pain is also mentioned while the person is sitting or driving a car. Usually there’s no acute trauma when the pain starts to appear, it gradually gets worse<ref name="13">Puranen J.; Orava S., The hamstring syndrome. A new diagnosis of gluteal sciatic pain, American Journal of Sports Medicine, 1988, 16(5): 517 – 521.
Level of evidence 4, grades of recommendation C</ref>. | ||
Continued exercises and stretching can cause even more pain<ref name="14">Migliorini S.; Merlo M.; Pricca P., The hamstring syndrome. Clinical and diagnostic features, etiology, and surgical management, J Sports Traumatol Relat Res 2000; 22: 86-92.
Level of evidence 4, grades of recommendation C</ref>.<br>Pain down the back of the thigh can be caused by irritation of the sciatic nerve. This nerve passes very close to the ischial tuberosity.<ref name="10" /> Due to its degenerative nature, this injury is classified as a tendinopathy rather than a tendonitis, an inflammatory pathology.<ref name="15">James Dunne, Proximal hamstring tendinopathy: a real pain in the butt for runners, Strength and rehab for endurance athletes
Available from: | Continued exercises and stretching can cause even more pain<ref name="14">Migliorini S.; Merlo M.; Pricca P., The hamstring syndrome. Clinical and diagnostic features, etiology, and surgical management, J Sports Traumatol Relat Res 2000; 22: 86-92.
Level of evidence 4, grades of recommendation C</ref>.<br>Pain down the back of the thigh can be caused by irritation of the sciatic nerve. This nerve passes very close to the ischial tuberosity.<ref name="10" /> Due to its degenerative nature, this injury is classified as a tendinopathy rather than a tendonitis, an inflammatory pathology.<ref name="15">James Dunne, Proximal hamstring tendinopathy: a real pain in the butt for runners, Strength and rehab for endurance athletes
Available from:http://www.kinetic-revolution.com/proximal-hamstring-tendinopathy-a-real-pain-in-the-butt-for-runners/ Level of evidence 3A, grades of recommendation B &amp;amp;amp;amp;amp;amp;amp;amp;amp; level of evidence 5, grades of recommendation D</ref> | ||
= | = Differential Diagnosis = | ||
First of all, it’s essential to determine if the pain is local or referred. If the patient says that the pain varies in location it will be referred pain. Pain in the buttock combined with pain in the lower back may refer to the lumbar spine. This may be caused by a problem with muscles, ligaments or disks. | First of all, it’s essential to determine if the pain is local or referred. If the patient says that the pain varies in location it will be referred pain. Pain in the buttock combined with pain in the lower back may refer to the lumbar spine. This may be caused by a problem with muscles, ligaments or disks. | ||
| Line 119: | Line 119: | ||
If the patient complains of higher pain (upper gluteal region) there might be a problem with the piriformis muscle.<br>Pain over the sacrum or near the sacroiliac joint refers to a pelvic stress fracture or inflammation or malalignment of the sacroiliac joint. There are also some uncommon cases where buttock and posterior thigh pain refer to chronic compartment syndrome of the posterior thigh. Due to the resemblance of some symptoms of this injury with other hip injuries, it’s important to get a proper diagnosis; this will likely entail a physical examination and an MRI.<ref name="4" /><br> | If the patient complains of higher pain (upper gluteal region) there might be a problem with the piriformis muscle.<br>Pain over the sacrum or near the sacroiliac joint refers to a pelvic stress fracture or inflammation or malalignment of the sacroiliac joint. There are also some uncommon cases where buttock and posterior thigh pain refer to chronic compartment syndrome of the posterior thigh. Due to the resemblance of some symptoms of this injury with other hip injuries, it’s important to get a proper diagnosis; this will likely entail a physical examination and an MRI.<ref name="4" /><br> | ||
= | = Diagnostic Procedures = | ||
An MRI is required to confirm the diagnosis and to take a look at the severity of the injury. <br>An MRI can recognize tendon thickening, tearing, inflammation and swelling at the tuber ishiadicum. You can also use ultrasound, but this technique isn’t able to give a precise visualization of bone marrow edema.<ref name="12">McCormack R. J., The management of bilateral high hamstring tendinopathy with ASTYM treatment and eccentric exercise: a case report, The Journal of Manual and Manipulative Therapy, 2012, 20(3) 142 – 146.
Level of evidence 4, grades of recommendation C</ref> <br>Normally a high hamstring injury may be combined with stress reaction or bone edema in the ischial tuberosity and findings of the tendon. In case of a tendinopathy an increased signal is noticeable on T1-weighted images with no abnormalities on fat-suppressed T2-weighted images.<ref name="4" /><ref name="5" /> | An MRI is required to confirm the diagnosis and to take a look at the severity of the injury. <br>An MRI can recognize tendon thickening, tearing, inflammation and swelling at the tuber ishiadicum. You can also use ultrasound, but this technique isn’t able to give a precise visualization of bone marrow edema.<ref name="12">McCormack R. J., The management of bilateral high hamstring tendinopathy with ASTYM treatment and eccentric exercise: a case report, The Journal of Manual and Manipulative Therapy, 2012, 20(3) 142 – 146.
Level of evidence 4, grades of recommendation C</ref> <br>Normally a high hamstring injury may be combined with stress reaction or bone edema in the ischial tuberosity and findings of the tendon. In case of a tendinopathy an increased signal is noticeable on T1-weighted images with no abnormalities on fat-suppressed T2-weighted images.<ref name="4" /><ref name="5" /> | ||
| Line 173: | Line 173: | ||
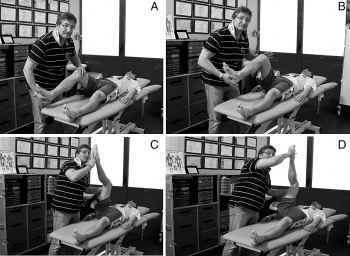
The test is performed while the patient is lying on his back. The hip and knee are maximally flexed. Slowly the therapist will straighten the knee till its maximal extension; the hip must remain in a 90° flexion. The test is also doable without the assistance of a therapist. The patient can use a rope or a belt to straighten his knee like depicted on the picture. | The test is performed while the patient is lying on his back. The hip and knee are maximally flexed. Slowly the therapist will straighten the knee till its maximal extension; the hip must remain in a 90° flexion. The test is also doable without the assistance of a therapist. The patient can use a rope or a belt to straighten his knee like depicted on the picture. | ||
{{#ev:youtube|Xg0ghED6AS8}}<ref>Physiotutors. Bent Knee Stretch Test ⎟ Proximal Hamstring Tightness and Tendinopathy. Available from: https://www.youtube.com/watch?v=Xg0ghED6AS8 </ref> | {{#ev:youtube|Xg0ghED6AS8}}<ref>Physiotutors. Bent Knee Stretch Test ⎟ Proximal Hamstring Tightness and Tendinopathy. Available from: https://www.youtube.com/watch?v=Xg0ghED6AS8 </ref> | ||
<br> | <br> | ||
<br>'''4) Modified bent-knee stretch test''' | <br>'''4) Modified bent-knee stretch test''' | ||
| Line 201: | Line 201: | ||
<br> | <br> | ||
The test is performed while the patient is lying on his back, the hip and knee are in extension. The therapist takes the heel in one hand and holds the knee with the other hand. He brings the hip and knee in maximal flexion and then rapidly straightens the knee.<br>These tests are used to identify a hamstrings origin tendinopathy, but do not replace an MRI.<ref name="10" / | The test is performed while the patient is lying on his back, the hip and knee are in extension. The therapist takes the heel in one hand and holds the knee with the other hand. He brings the hip and knee in maximal flexion and then rapidly straightens the knee.<br>These tests are used to identify a hamstrings origin tendinopathy, but do not replace an MRI.<ref name="10" /> | ||
= | = Prevention = | ||
A good flexibility of the hamstring and quadriceps muscles is a good prevention for this injury.<br>Some preventive techniques related to sport and hamstring injuries are to avoid block drills in the beginning of the season or on two following days.<ref name="2">Fu F.H. and Stone D.A., 1994 Sports injuries: mechanisms, prevention, and treatment. Baltimore: Williams &amp;amp;amp;amp;amp;amp;amp; Wilkins. Pp. 654.
Level of evidence 3A, grades of recommendation B</ref> <br><br> | A good flexibility of the hamstring and quadriceps muscles is a good prevention for this injury.<br>Some preventive techniques related to sport and hamstring injuries are to avoid block drills in the beginning of the season or on two following days.<ref name="2">Fu F.H. and Stone D.A., 1994 Sports injuries: mechanisms, prevention, and treatment. Baltimore: Williams &amp;amp;amp;amp;amp;amp;amp;amp; Wilkins. Pp. 654.
Level of evidence 3A, grades of recommendation B</ref> <br><br> | ||
= <br>Medical Management = | = <br>Medical Management = | ||
| Line 225: | Line 225: | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
<div class="researchbox">
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=14spTIXMx9q9VwGc_iFE1h7hwFbE0SyCjyPXH6byN8-VfyckEt|charset=UTF8|short|max=10</rss>
<br> </div> | <div class="researchbox">
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=14spTIXMx9q9VwGc_iFE1h7hwFbE0SyCjyPXH6byN8-VfyckEt|charset=UTF8|short|max=10</rss>
<br> </div> | ||
= | |||
= References = | |||
<references /><br> | <references /><br> | ||
[[Category: | [[Category:Conditions]] [[Category:Knee]] [[Category:Hip]] [[Category:Knee_Conditions]] [[Category:Sports_Injuries]] [[Category:Musculoskeletal/Orthopaedics]] | ||
Revision as of 08:44, 26 May 2017
Original Editor - Melissa De Maeyer
Top Contributors - Wanda van Niekerk, Kim Jackson, Vidya Acharya, Mandeepa Kumawat, Mariam Hashem, Lisa De Donder, Melissa De Maeyer, Vanessa Rhule, Lotte De Clerck, Admin, WikiSysop, 127.0.0.1, Oyemi Sillo, Rachael Lowe, HaniaElGibaly, Evan Thomas, Naomi O'Reilly, George Prudden and Kai A. Sigel
Description[edit | edit source]
Hamstring origin tendinopathy, also called proximal hamstring tendinopathy or high hamstring tendinopathy, are a group of pathologies of the proximal hamstring tendon. They contain tendon degeneration, partial tearing and peritendinous inflammatory reaction.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Clinically Relevant Anatomy[edit | edit source]
One of the most important muscle groups in running is the hamstring. They are active at multiple points in the gait cycle, namely the knee flexion and the hip extension.
The distal attachment is located on the top of your tibia, just behind the knee. The origin is divided in three branches, one starting from the femur and the two remaining ones starting from the ischial tuberosity. The junction between the tendons of the hamstrings and the ischial tuberosity is the area affected by high hamstring tendinopathy. The tendon’s thickness, fibrousness and poor blood supply is the cause of a difficult healing.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
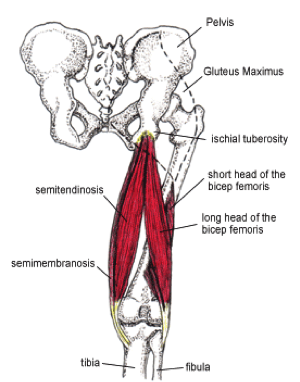
The muscles of the hamstrings have a higher proportion of type 2 muscle fibers than the other muscles of the lower extremity. This suggests that these muscles can generate high intrinsic tension force. While running, the time increases that the hamstrings are under maximal stretch. The hamstrings and their tendon attachments have to endure heavy charges or high tensions because of these two forces, namely during eccentric contractions.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
(For extra information about pathology mechanisms see Tendinopathy)
Epidemiology / Etiology[edit | edit source]
Hamstring origin tendinopathy may arise after an acute tear at the origin that is not adequately treated. Still in most cases it’s a common overuse injury that is often seen in runners (more in middle- or long-distance runners than sprinters). It typically occurs with repetitive jumping, kicking and running activities. The hamstrings are prone to this type of injury as they contribute to the decelerating of the extension of the knee during activities such as sprinting and hill climbing. (Petersen J. et al, 2005)
The following factors can also increase the risk of hamstring origin tendinopathy:
Intrinsic factors:
- Malalignments
- Leg length discrepancy
- Imbalance
- Decreased flexibility
A study of stretching found that there are more hamstring problems with persons who didn’t stretch before participating in sports.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Joint laxity
- Female gender
- Age - When you get older, there is a reduction in muscle fiber size and number. This leads to a loss of mass and strength.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Overweight
- Proprioceptive weakness[1]
- Ischial tuberosity tenderness
- Core weakness
- Pelvic dysfunction[2]
- Previous injury - the strength is reduced by previous hamstrings, knee or groin injuries.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Neuromyofascial involvement- there is an increased neural tension and posterior thigh pain. There can be myofascial trigger points; this is associated with a decrease of flexibility.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Stiffness of the hip
- Tightness/Weakness of the hamstrings and quadriceps
- Bad pelvic/core stability.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Extrinsic factors:
- excessive, repetitive load on the body
- training errors,
- environmental malconditions
- poor equipment
- Insufficient warming up - A warm-up with isometric contractions increases strength and length of the muscle.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Excessive training
- Fatigue - The muscle has less energy. There is also a lack of concentration, coordination and technique.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Apparently core weakness and pelvic dysfunction seem to be closely related to the development of a hamstring tendinopathy.[2] The tendinopathy usually starts with micro-damage without a remarkable trauma. Normally the tendon is capable to intrinsic repair, meaning that the consequences of this injury are little. Sometimes, imbalance can cause further damage and failed healing. All of this leads to the formation of tendinosis. (Kannus 1997, Sharma and Maffulli 2005, Warden 2007.) Intrinsic and extrinsic factors contribute to the formation of this injury.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Characteristics / Symptoms[edit | edit source]
Hamstring origin tendinopathy is related with deep buttock pain and pain in the posterior thigh. The pain is often felt in the lower gluteal region, radiating along the hamstings[2].
The pain increases while repetitive activity (such as long-distance running) and in worse cases pain is also mentioned while the person is sitting or driving a car. Usually there’s no acute trauma when the pain starts to appear, it gradually gets worseCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Continued exercises and stretching can cause even more painCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Pain down the back of the thigh can be caused by irritation of the sciatic nerve. This nerve passes very close to the ischial tuberosity.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Due to its degenerative nature, this injury is classified as a tendinopathy rather than a tendonitis, an inflammatory pathology.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Differential Diagnosis[edit | edit source]
First of all, it’s essential to determine if the pain is local or referred. If the patient says that the pain varies in location it will be referred pain. Pain in the buttock combined with pain in the lower back may refer to the lumbar spine. This may be caused by a problem with muscles, ligaments or disks.
If the pain is more local and constant it’s a pathology in the buttock itself. If the pain is located near the ischial tuberosity it may represent to hamstring origin tendinopathy or also ischiogluteal bursitis.
If the patient complains of higher pain (upper gluteal region) there might be a problem with the piriformis muscle.
Pain over the sacrum or near the sacroiliac joint refers to a pelvic stress fracture or inflammation or malalignment of the sacroiliac joint. There are also some uncommon cases where buttock and posterior thigh pain refer to chronic compartment syndrome of the posterior thigh. Due to the resemblance of some symptoms of this injury with other hip injuries, it’s important to get a proper diagnosis; this will likely entail a physical examination and an MRI.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Diagnostic Procedures[edit | edit source]
An MRI is required to confirm the diagnosis and to take a look at the severity of the injury.
An MRI can recognize tendon thickening, tearing, inflammation and swelling at the tuber ishiadicum. You can also use ultrasound, but this technique isn’t able to give a precise visualization of bone marrow edema.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Normally a high hamstring injury may be combined with stress reaction or bone edema in the ischial tuberosity and findings of the tendon. In case of a tendinopathy an increased signal is noticeable on T1-weighted images with no abnormalities on fat-suppressed T2-weighted images.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
However a series of provocation tests have been developed in order to help for the diagnose of this injury.
Pain provocation tests:
1) Palpation of the tuber ishiadicum
2) The Puranen-Orava test
This test is a standing stretch of the hamstrings, there must be a hip flexion of 90°. The foot rests on a support and the knee is in extension.
3) Bent-knee stretch test:
The test is performed while the patient is lying on his back. The hip and knee are maximally flexed. Slowly the therapist will straighten the knee till its maximal extension; the hip must remain in a 90° flexion. The test is also doable without the assistance of a therapist. The patient can use a rope or a belt to straighten his knee like depicted on the picture.
4) Modified bent-knee stretch test
The test is performed while the patient is lying on his back, the hip and knee are in extension. The therapist takes the heel in one hand and holds the knee with the other hand. He brings the hip and knee in maximal flexion and then rapidly straightens the knee.
These tests are used to identify a hamstrings origin tendinopathy, but do not replace an MRI.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Prevention[edit | edit source]
A good flexibility of the hamstring and quadriceps muscles is a good prevention for this injury.
Some preventive techniques related to sport and hamstring injuries are to avoid block drills in the beginning of the season or on two following days.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Medical Management[edit | edit source]
Anti-inflammatory drugs can help to deliver the irritated tissue around the tendon.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
In more severe cases, when physical therapy does not help, a corticosteroid injection into the peritendinous soft tissues is recommended, injecting the substance in the tendon itself can be dangerous. It’s important to know that this does not replace the therapy but it’s a part of the therapy. However, corticosteroid injections can also have a negative impact on the tendons inter alia the weakening of tendons, the rupture of tendons, particularly in load-bearing tendons (Kleinman M. et al, 1983). Frederickson et al. found that patients whose MRIs showed more swelling around the tuberositas ischiadicum and less thickening of the tendon got more relief from a cortisone injection than patients with more pronounced tendon thickening. A novel treatment is platelet-rich plasma injection at the origin of the muscle.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Platelet-rich plasma (PRP) seems to be a promising alternative to the corticosteroid injections. The alpha and dense granulates that are present in the platelets, release multiple growth factors and cytokines that promote wound healing (Alsousou J. et al, 2009 & Mishra A. et al, 2009). An enhancement of the recruitment, proliferation and differentiation of the cells involved in soft-tissue regeneration has been reported by the authors of in vitro studies (Hall MP et al, 2009, De Mos M. et al, 2008)
The shockwave therapy has almost no influence on hamstrings origin tendinopathies.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
When the conservative therapy doesn’t work, the patients need surgery to decrease the pressure on the nerve and to divide the fibrous and damaged tendon.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Physical Therapy Management[edit | edit source]
When a patient is diagnosed with hamstring origin tendinopathy, it’s usually preferable to consult a physical therapist. The earlier he starts with a physiotherapy treatment the faster he’ll return to his normal function. Normally this will take a couple of weeks but sometimes, when a patient has had hamstring origin tendinopathy for a longer period, it may take months to recover.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The first thing a physical therapist will have to do is trying to control the pain. This occurs with ice, electrical stimulation of the tendon and pulsed ultrasound.
In the beginning of the treatment a misalignment of the pelvis has to be corrected because this might increase the tension in the hamstring muscles. It can also cause a decreased strength of the muscles. This misalignment is usually an anterior tilt of the pelvis and can easily be corrected by manual or chiropractic manipulation.
Soft-tissue mobilization has to be included in the rehabilitation program. It’s very beneficial to break up the adhesions and scar tissues. A friction treatment with transverse frictions is commonly used. The therapist has to pay attention to not compress directly the ischial tuberosity as it can irritate underlying edema. Techniques like ART (Active Release Technique) or Gastron can be included as well.
At the same time the patient may start a gradually built up stretching program for the hamstrings. This is also a crucial step in the process. Both legs should be stretched to have some balance. Even the antagonist hip-flexor muscles should be stretched for an optimal function. The RoM can be increased by the use of ultrasound or shockwave therapy before stretching. Frequent stretching may avoid a reappearance of the injury.
It’s important to regain strength in the muscle. First it’s best to begin with double-leg non weight-bearing isometric exercises followed by single-leg closed-chain isometrics and isotonic open-chain exercises. A good treatment for tendinopathies is an eccentric muscle strengthening program. This can normalize the thickness and structure of the tendon. It can also prepare the hamstrings for the high-force load while running. Glute bridges are interesting exercises to start a strength rehabilitation program with. Afterwards the patient can start with introductory exercises such as a standing ‘hamstring catch’. By using a Swiss Ball we can increase the difficulty of the exercise. As Frederickson et al stated, Swiss ball curl is ideal for development of both eccentric and concentric strength. According to the tolerance and the progression of the patient these Swiss ball curls can be practiced with short range of motion to full range of motion and eventually, single-legged Swiss ball curls.
Another point that must not be neglected is the importance of core strength. Core strength is a considerable element for the rehabilitation of hamstring origin tendinopathy as it reduces the risk of recurrent hamstring strains. As stated above a misalignment of the pelvis has to be corrected. By reinforcing the musculature of the abdomen and the hip the pelvis can be stabilized, taking strain of the hamstring. Plank exercises, especially with leg lifts incorporated are recommended by Frederickson who has conducted numerous studies about the rehabilitation of the hamstrings. Exercises like these encourage co-activation of the glute and hamstring muscles.
The previously mentioned exercises are considered as conservative treatments. More aggressive treatments are the ones including medical treatment such as injections or even surgery (see: Medical Management). Surgery is recommended for a resistance towards the conservative treatment. According to Puranen et al‘s study satisfactory results can often be expected. The main purpose of this intervention is to relieve tension on the sciatic nerve. As showed in the study of Lempainen (2009) the majority of the athletes are able to return to the same level of sport after receiving surgery of a high hamstring tendinopathy. As this sounds encouraging we must keep in mind that the average recovery time of five months is a quite long period when it comes to time off from running.[4]
If the RoM of the muscle is normal and pain-free, pool running and stationary biking could be put into the rehabilitation program.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Running again:
High hamstring tendinopathy is known as a disease that takes a long time to recover from. Fredericson et al. estimates a recovery of 8-12 weeks. It’s likely that cross training doesn’t stress the legs until the bent-knee stretch test can be done without pain.
The moment that you can do the exercise shown on the picture below, you can begin with the return-to-running program described here:
Week 1: Walk 5min/jog 1min, build to sets on alternating days (ex. 2x5min/1min, off, 3x5min/1min, off, ect)
Week 2: If no pain, walk 5min/jog 5min, build to 5 sets on alternating days
Week 3: If no pain, advance to 20min jog, no more than 5 days per week
Week 4: If no pain, advance to 20min run at normal training pace, no more than 5 days per week
Week 5-8: If no pain, gradually increase running speed, volume, and acceleration as tolaretedCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ White, K. E., High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine 2011, 10 (2), 93-99 Level of evidence 4. grades of recommendation C
- ↑ 2.0 2.1 2.2 Fredericson, M.; Moore, W.; Guillet, M.; Beaulieu, C., High hamstring tendinopathy in runners: Meeting the challanges of diagnosis, treatment, and rehabilitation. Physician and Sportsmedicine 2005, 33 (5), 32-43. Level of evidence 4, grades of recommendation C
- ↑ Physiotutors. Bent Knee Stretch Test ⎟ Proximal Hamstring Tightness and Tendinopathy. Available from: https://www.youtube.com/watch?v=Xg0ghED6AS8
- ↑ Lempainen, L.; Sarimo, J.; Mattila, K.; Vaittinen, S.; Orava, S., Proximal Hamstring Tendinopathy: Results of Surgical Management and Histopathologic Findings. The American Journal of Sports Medicine 2009, 37 (4), 727-734. Level of evidence 3A, grades of recommendation B