Hallux Rigidus: Difference between revisions
No edit summary |
No edit summary |
||
| Line 113: | Line 113: | ||
'''Mann and Clanton<ref name="Mann and Clanton" />''' | '''Mann and Clanton<ref name="Mann and Clanton" />''' | ||
Cheilectomy was performed on the distal part of the first metatarsal of twenty-five patients who had hallux rigidus. Relief of pain was achieved in all but three patients, whose cases were considered as failures. Joint motion improved by an average of 20 degrees, and it was in an acceptable range in twenty-three patients. There were no complications other than persistence of swelling in six patients. No patient required additional operative intervention during an average follow-up of fifty-six months. The authors concluded that cheilectomy is a better method of treatment for hallux rigidus than arthrodesis, resection arthroplasty, or arthroplasty with the use of a flexible implant. <br><br>'''Gould N<ref>Gould N. Foot &amp;amp;amp;amp;amp;amp;amp;amp;amp; Ankle.1981 May; 1(6):315-20.</ref>''' | Cheilectomy was performed on the distal part of the first metatarsal of twenty-five patients who had hallux rigidus. Relief of pain was achieved in all but three patients, whose cases were considered as failures. Joint motion improved by an average of 20 degrees, and it was in an acceptable range in twenty-three patients. There were no complications other than persistence of swelling in six patients. No patient required additional operative intervention during an average follow-up of fifty-six months. The authors concluded that cheilectomy is a better method of treatment for hallux rigidus than arthrodesis, resection arthroplasty, or arthroplasty with the use of a flexible implant. <br><br>'''Gould N<ref>Gould N. Foot &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Ankle.1981 May; 1(6):315-20.</ref>''' | ||
Fifty-one feet in 42 patients with varying degrees of symptomatic hallux rigidus and with 2 years of follow-up were operated with excellent results. Cheilotomy was performed in all cases with only cheilotomy employed in the young patients and implant surgery (single-stem silicone) reserved for the older and more advanced arthritis cases. Pain generally disappeared within 3 months. Range of toe motion in dorsiflexion increased. All patients returned to their activity of choice. All patients were able to utilize off-the-shelf footwear post-operatively. <br> | Fifty-one feet in 42 patients with varying degrees of symptomatic hallux rigidus and with 2 years of follow-up were operated with excellent results. Cheilotomy was performed in all cases with only cheilotomy employed in the young patients and implant surgery (single-stem silicone) reserved for the older and more advanced arthritis cases. Pain generally disappeared within 3 months. Range of toe motion in dorsiflexion increased. All patients returned to their activity of choice. All patients were able to utilize off-the-shelf footwear post-operatively. <br> | ||
| Line 151: | Line 151: | ||
<references /><br> | <references /><br> | ||
[[Category:Foot]][[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | [[Category:Foot]][[Category:Musculoskeletal/Orthopaedics|Orthopaedics]][[Category:Foot_and_Ankle_Conditions]] | ||
Revision as of 12:51, 29 March 2017
Original Editor - Tracy Hall
Top Contributors - Admin, Ewa Jaraczewska, Rachael Lowe, Jess Bell, Tracy Hall, Laura Ritchie, Kim Jackson, Ilse De Bode, Simisola Ajeyalemi and Khloud Shreif
Clinically Relevant Anatomy
[edit | edit source]
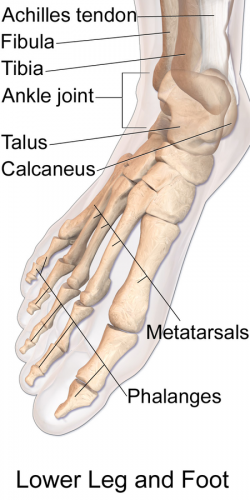
Hallux rigidus is a condition affecting the first metatarsophalangeal (MTP) joint of the big toe or great toe. The base of the the first MTP specifically is where the degenerative arthritis is typically found. The joint is covered with articular cartilage, a shiny covering to protect the ends of the bones within the joint. As this covering wears, degeneration occurs until bone is against bone. Bone spurs develop as part of this degenerative process and movement decreases. Normal range of motion is between 65 to 100 degrees.
|
[1] |
Mechanism of Injury / Pathological Process
[edit | edit source]
Hallux Rigidus is a progressive disorder. The toe’s motion is decreased over time. Some causes are faulty function or biomechanics and structural abnormalities. Wear and tear over time can lead to osteoarthritis in the joint.
Clinical Presentation[edit | edit source]
Pain, stiffness and loss of motion are the some signs of hallux rigidus. Burning pain and paraesthesia can be present. Walking, standing and wearing heels aggravate the pain. Symptoms are relieved by rest.
The normal dorsiflexion range of motion of the first MTP joint is at least 65 degrees[2][3][4][5]. Nawoczenski, et al[6] showed a new standard of “normal” range of dorsiflexion range of motion of the great toe joint should now be set at approximately 45 degrees. However, this dorsiflexion range has only been verified for walking gait, not running.
Diagnostic Procedures[edit | edit source]
Weight bearing, anterior posterior and lateral radiographs are usually needed to examine the joint. Often non-uniform joint space narrowing, widening or flattening of the 1st MT head is seen. Subchondral sclerosis or cysts, horseshoe shaped osteophytes, lateral greater than medial osteophytes and sesamoid hypertrophy may be seen.
A clinical/radiographic grading system was described by Regnauld and appears mainly in the European literature.
Hattrup and Johnson[7] described a radiographic classification which has become standard, and in fact correlates quite well with the Regnauld grading:
- Grade 1: mild to moderate osteophytes formation but good joint space preservation
- Grade 2: moderate osteophyte formation with joint space narrowing and subchondral sclerosis
- Grade 3: marked osteophyte formation and loss of the visible joint space, with or without subchondral cyst formation
Coughlin et al[8] modified the Hattrup and Johnson classification to create the Coughlin and Shurnass[9] classification:
- Grade 0:
- Dorsiflexion 40-60°
- Normal radiography
- No pain
- Grade 1
- Dorsiflexion 30-40°
- Dorsal osteophytes
- Minimal/ no other joint changes
- Grade 2
- Dorsiflexion 10-30°
- Mild to moderate joint narrowing or sclerosis
- Osteophytes
- Grade 3
- Dorsiflexion less than 10°
- Severe radiographic changes
- Constant moderate to severe pain at extremities
- Grade 4
- Stiff joint
- Severe changes with loose bodies and osteochondritis dissecans
Examination
[edit | edit source]
Look for other features of systemic arthropathy. Assess the overall foot shape, range of ankle dorsiflexion and function of the other foot joints Identify sites of tenderness – is the osteophyte symptomatic?
Evaluate the severity of rigidity and the residual arc of movement Is pain provoked mainly by dorsiflexion, plantarflexion or throughout the range of movement?
Check the alignment of the great toe, looking for IPJ hyperextension or hallux rigidus with valgus Are there any lesser ray problems?
Outcome Measures[edit | edit source]
Visual analog scales, AOFAS (American Orthopaedic Foot and Ankle Society) scores, Subjective self assessment score, MTP dorsiflexion, MTP total motion and presentation of callus are examined
Management / Interventions
[edit | edit source]
Nonsurgical or conservative approaches:[edit | edit source]
Treatment for mild or moderate causes of Hallux rigidus includes anti-inflammatory NSAIDS medications that are often prescribed and usually start to relieve some symptoms with in three to four days. Glucosamine chondrointin sulfate, vitamins and minerals are recommended. Molded stiff inserts with rigid bar or rocker bottom shoes usually begin to help with in a few weeks. Shoes with a large toe box and cessation of high heels , kneeling or excessive squatting may help. Cortisone injections give relief with in 24 hours but often are only temporary.
Physical therapy to provide joint mobilizations, manipulation , range of motion, muscle reeducation, strengthening of the flexor hallucis longus muscles as well as the plantar intrinsics muscles of the feet can improve stability of the 1st MTP. Gait training for stage 1 and 2 (protection, rest, ice, compression and elevation) is often helpful to reduce the inflammation during initial stages. All of these measures can be of value to the patient even if he or she ultimately undergoes surgery.
Runners with stage II and greater hallux rigidus may need to switch to lightweight day hikers and switch from asphalt to dirt trails for long distance running.
The primary goal of foot orthotic therapy or shoe modification should be blocking or shielding the hallux from dorsiflexion at the first metatarsal.
The indication for surgery was intractable pain isolated to the first metatarsophalangeal joint that was refractory to shoe
modifications, use of rigid shoe inserts, nonsteroidal anti-inflammatory medications, and modification of activities.
| [10] | [11] |
Surgical therapy:
[edit | edit source]
The indication for surgery is intractable pain isolated to the first metatarsophalangeal joint that is refractory to shoe modification, use of rigid shoe inserts, nonsteroidal anti-inflammatory medications, and modification of activities. Choice depends on the stage of involvement, the limitations in range of motion, the activity level of the patient and the preferences of the surgeon and patient.
Types of surgery include:
- Cheiloectomy - A procedure to remove bone spurs at the top of the joint allowing greater toe extension and improved walking. Usually beneficial for mild to moderate disease with less than 50% of joint affected usually grade 1 and grade 2[12].
- Dorsiflexion phalangeal osteotomy - In patients with a reasonable range of motion, a dorsal wedge osteotomy of the phalanx increases dorsiflexion at a theoretical cost of loss of plantar flexion. Mild to moderate cases occasionally require this procedure.
- Metatarsal Osteotomy – a slice is removed from the dorsal limb to slide the head down and proximally. The Place for these procedures is uncertain and more complex than cheilectomies. These procedures are intended for use in early hallux rigidus
- Excision Arthroplasty or Keller procedure[13] - The Keller procedure is when resection of the base of the proximal phalanx and soft-tissue reconstruction is performed with the intention to decompress the joint and improve pain and range of movement. The Keller procedure may lead to great toe weakness, cock-up deformity and metatarsalgia[14].
- MTP Arthrodesis - This is a procedure is performed to fuse the joint surfaces and is a favored procedure. Suitable for most cases and severity but usually grades 3 and 4 are recommended .Suitable as salvage when other procedures have failed (for example Keller procedure) Arthrodesis of the first MPJ consistently show superior results and patient satisfaction in comparison to other surgical options. While cheilectomy may be beneficial for early stages of hallux rigidus, arthrodesis of the first MPJ appears to be the best option for the relief of symptoms with stage III and stage IV hallux rigidus in active, athletic patients. A randomized controlled trial by O’Doherty et al[15] found no difference in functional outcome between arthrodesis and Keller arthroplasty in 81 patients over the age of 45 (some of whom had hallux valgus in addition to OA). Fusion remains the gold standard for the management of end-stage hallux rigidus; it is cheaper and simpler than arthroplasty and no study has yet shown advantage for the extra cost.
- Artificial joint replacement - A procedure to replace joint surfaces with a plastic or metal surface. The downside to this is the joint may not last a life time and there is currently no study documenting the long-term performance of any first MTP joint prosthesis in running athletes
Differential Diagnosis
[edit | edit source]
Turf toe, fracture, gout, rheumatoid arthritis could be some other causes of pain and stiffness in the 1st MTP joint.
Key Evidence[edit | edit source]
Hattrup and Johnson[7]
The records of 58 patients who had hallux rigidus and were treated with cheilectomy between 1977 and 1984 showed the following results: 53.4% completely satisfactory, 19% mostly satisfactory, 27.6% unsatisfactory. No deterioration of results with time was apparent. When the results were analyzed in relation to the degenerative changes that were evident in the preoperative roentgenograms, the failure rate was increased from 15% with Grade I changes to 37.5% with Grade III changes. The authors conclude that cheilectomy is the procedure of choice in patients with hallux rigidus and Grade I changes.
Mann and Clanton[12]
Cheilectomy was performed on the distal part of the first metatarsal of twenty-five patients who had hallux rigidus. Relief of pain was achieved in all but three patients, whose cases were considered as failures. Joint motion improved by an average of 20 degrees, and it was in an acceptable range in twenty-three patients. There were no complications other than persistence of swelling in six patients. No patient required additional operative intervention during an average follow-up of fifty-six months. The authors concluded that cheilectomy is a better method of treatment for hallux rigidus than arthrodesis, resection arthroplasty, or arthroplasty with the use of a flexible implant.
Gould N[16]
Fifty-one feet in 42 patients with varying degrees of symptomatic hallux rigidus and with 2 years of follow-up were operated with excellent results. Cheilotomy was performed in all cases with only cheilotomy employed in the young patients and implant surgery (single-stem silicone) reserved for the older and more advanced arthritis cases. Pain generally disappeared within 3 months. Range of toe motion in dorsiflexion increased. All patients returned to their activity of choice. All patients were able to utilize off-the-shelf footwear post-operatively.
Coughlin and Shurnas [17]
This long-term study over 1 nineteen year period documents and evaluates the outcome of surgical treatment of hallux rigidus in ones surgeon’s practice. The authors concluded that cheilectomy was used with predictable success to treat Grade-1 and 2 and selected Grade-3 cases. Patients with Grade-4 hallux rigidus or Grade-3 hallux rigidus with <50% of the metatarsal head cartilage remaining at the time of surgery should be treated with arthrodesis. For patients who desire preservation of motion and are willing to accept less than total pain relief, cheilectomy provides a high proportion of good and excellent long-term results. However, arthrodesis should be considered for patients who clearly have pain in the mid-range of motion on examination. A high proportion of these patients can be expected to have a good or excellent long-term result
Coughlin MJ, Shurnas PJ[18]
Seven patients (seven feet) were evaluated at an average follow-up of 42 months following soft-tissue interposition arthroplasty of the hallux metatarsophalangeal (MTP) joint for severe hallux rigidus. This technique of soft-tissue interposition arthroplasty gave excellent pain relief and reliable function of the hallux, and is an alternative treatment to MTP arthrodesis in select cases of severe hallux rigidus.
Brodsky JW, Baum BS, Pollo FE, Mehta H[19].
A prospective gait analysis study was performed on 23 patients with symptomatic hallux rigidus to objectively evaluate the effects of first MTP joint arthrodesis on gait. They were seen at an average of 8.6 days before surgery and then again at least 1 year post-operatively. There were three statistically significant changes in gait: increases in maximal ankle push-off power and single-limb support time on the involved extremity, and a decrease in step width. The authors concluded that first MTP joint arthrodesis produces objective improvement in propulsive power, weight-bearing function of the foot, and stability during gait.
Case Studies[edit | edit source]
Nawoczenski DA - Case study of the management of an individual with hallux rigidus deformity[20]
The objective of the study was to describe the outcome of nonoperative and operative treatment, including kinematic and kinetic changes following cheilectomy surgery, for an individual with hallux rigidus deformity. The patient was a 54-year-old man who sustained a traumatic injury to the great toe. Conservative treatment included nonsteroidal anti-inflammatory drugs, custom insole fabrication, and footwear outersole modification. Because of continued pain, loss of motion, and restrictions in daily activities, the patient elected to have surgery, and a cheilectomy procedure was done. The outcome of surgery proved favorable, both subjectively and objectively. Peak dorsiflexion increased significantly (a minimum of 20 degrees) for all clinical tests and walking trials at the first metatarsophalangeal joint when compared with preoperative measurements. Peak plantar pressures also increased over the medial forefoot (68%) and hallux (247%) between preoperative testing and follow-up, indicating increased loading to this region of the foot. The study suggests that restrictions in motion and daily activities and persistent pain may warrant surgical intervention for individuals with hallux rigidus deformity.
Resources
[edit | edit source]
Richie D. How To Treat Hallux Rigidus In Runners. 4 April 2009. Available from: www.podiatrytoday.com/how-to-treat-hallux-rigidus-in-runners. [last accessed 5/6/9]
Foot and Ankle Center of Washington, Seattle. Available at www.footankle.com/Hallux-Rigidus.htm [last accessed 24/5/9].
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1TcjM2U847OptqcDUk4M6Nw2d4wo3W2UcBQVAie4_6TT7XMAV|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ SLO Motion Shoes. Hallux Rigidus: Causes, Diagnosis, and Treatment. Available from: http://www.youtube.com/watch?v=umCSpwEvWUM [last accessed 06/01/17]
- ↑ Root ML, Orien WP, Weed JH. Normal and abnormal function of the foot. In Clinical Biomechanics, vol II, Clinical Biomechanics Corp., Los Angeles, 1977
- ↑ Buell T, Green D, Risser J. Measurement of the first metatarsophalangeal joint range of motion. JAPMA 78:439, 1988.
- ↑ Bojsen-Moller F, Lamoreux L. Significance of free dorsiflexion of the toes in walking. Acta Orthop Scand 50: 471, 1979
- ↑ Hetherington VJ, Johnson RE, Albritton JS. Necessary dorsiflexion of the first metatarsophalangeal joint during gait. J Foot Surg 29:218, 1990
- ↑ Nawoczenski DA, Baumhauer JF, Umberger BR. Relationship between clinical measurements and motion of the first metatarsophangeal joint during gait. J Bone Joint Surg 81(3): 370-6, 1999.
- ↑ 7.0 7.1 Hattrup SJ, Johnson KA. Subjective results of hallux rigidus following treatment with cheilectomy. Clin Orthop 1988;226:182-91
- ↑ Coughlin MJ et al. Hallux rigidus. JBJS 2003; 85A:2072-88
- ↑ Coughlin MJ and Shurnas PS. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int 2003; 24(10): 731-43.
- ↑ Correct Toes. Spread Your Toes™ Series: Hallux Limitus Conservative Care vs. Conventional Care. Available from: http://www.youtube.com/watch?v=iTFn1Ldq1G8 [last accessed 06/01/17]
- ↑ Joan Hope Craig. Functional hallux mobilization. Available from: http://www.youtube.com/watch?v=ZOur5I0RTVo [last accessed 06/01/17]
- ↑ 12.0 12.1 Mann RA, Clanton TO. Hallux rigidus: treatment by cheilectomy. J Bone Jt Surg 1988; 70A:400-6
- ↑ Keller's arthroplasty. J Bone Jt Surg 1990; 72B:839-42
- ↑ Blewett N, Greiss ME. Long-term outcomes following Keller’s excision arthroplasty of the great toe. Foot 1993; 3:144-7
- ↑ DP O'Doherty, IG Lowrie, PA Magnussen, and PJ Gregg. The management of the painful first metatarsophalangeal joint in the older patient. Arthrodesis or Keller's arthroplasty? Journal of Bone and Joint Surgery - British Volume, 72-B(5), 839-842
- ↑ Gould N. Foot &amp;amp;amp;amp;amp;amp;amp;amp;amp; Ankle.1981 May; 1(6):315-20.
- ↑ Michael J. Coughlin and Paul S. Shurnas. Hallux Rigidus. Grading and Long-Term Results of Operative Treatment. J. Bone Joint Surg. Am., Nov 2003; 85: 2072 - 2088.
- ↑ Coughlin MJ, Shurnas PJ. Soft-tissue arthroplasty for hallux rigidus. Foot Ankle International. 2003 Sep;24(9):661-72.
- ↑ Brodsky JW, Baum BS, Pollo FE, Mehta H. Prospective gait analysis in patients with first metatarsophalangeal joint arthrodesis for hallux rigidus. Foot Ankle International. 2007 Feb;28(2):162-5
- ↑ Nawoczenski DA. Nonoperative and operative intervention for hallux rigidus. J Othrop Sports Phys Ther. 1999 Dec;29(12):727-35.







