Foot and Ankle Ability Measure: Difference between revisions
Evan Thomas (talk | contribs) mNo edit summary |
Evan Thomas (talk | contribs) mNo edit summary |
||
| Line 2: | Line 2: | ||
'''Original Editors''' - [[User:Niels Verbeeck|Niels Verbeeck]] | '''Original Editors''' - [[User:Niels Verbeeck|Niels Verbeeck]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Intended Population<ref name="1">Martin RL, Hutt DM, Wukich DK. Validity of the Foot and Ankle Ability Measure (FAAM) in Diabetes Mellitus. Foot Ankle Int. 2009 Apr;30(4):297-302</ref><ref name="2">Walmsley et al. The rheumatoid foot: a systematic literature review of patient-reported outcome measures. Journal of Foot and Ankle Research 2010, 3:12.</ref><ref name="3">RobRoy L. Martin. Evidence of Validity for the Foot and Ankle Ability Measure (FAAM). 2005</ref><ref name="4">Eechaute et al. The clinimetric qualities of patient-assessed instruments for measuring chronic ankle instability: A systematic review. BMC Musculoskeletal Disorders 2007, 8:6 doi:10.1186/1471-2474-8-6.</ref><ref name="5">Christopher R. Carcia et al. Validity of the Foot and Ankle Ability Measure in Athletes With Chronic Ankle Instability. Journal of Athletic Training 2008;43(2):179–183.</ref><ref name="6">RobRoy L. Martin. A Survey of Self-reported Outcome Instruments for the Foot and Ankle. Journal of orthopaedic sports physical therapy. 2007.</ref><ref name="7">Stephane Borloz et al. Evidence for Validity and Reliability of a French Version of the FAAM. BMC Musculoskeletal Disorders 2011, 12:40doi:10.1186/1471-2474-12-40.</ref> == | == Intended Population<ref name="1">Martin RL, Hutt DM, Wukich DK. Validity of the Foot and Ankle Ability Measure (FAAM) in Diabetes Mellitus. Foot Ankle Int. 2009 Apr;30(4):297-302</ref><ref name="2">Walmsley et al. The rheumatoid foot: a systematic literature review of patient-reported outcome measures. Journal of Foot and Ankle Research 2010, 3:12.</ref><ref name="3">RobRoy L. Martin. Evidence of Validity for the Foot and Ankle Ability Measure (FAAM). 2005</ref><ref name="4">Eechaute et al. The clinimetric qualities of patient-assessed instruments for measuring chronic ankle instability: A systematic review. BMC Musculoskeletal Disorders 2007, 8:6 doi:10.1186/1471-2474-8-6.</ref><ref name="5">Christopher R. Carcia et al. Validity of the Foot and Ankle Ability Measure in Athletes With Chronic Ankle Instability. Journal of Athletic Training 2008;43(2):179–183.</ref><ref name="6">RobRoy L. Martin. A Survey of Self-reported Outcome Instruments for the Foot and Ankle. Journal of orthopaedic sports physical therapy. 2007.</ref><ref name="7">Stephane Borloz et al. Evidence for Validity and Reliability of a French Version of the FAAM. BMC Musculoskeletal Disorders 2011, 12:40doi:10.1186/1471-2474-12-40.</ref> == | ||
| Line 52: | Line 53: | ||
As well the ADL subscale as the Sport subscale of the FAAM were sensitive to significant changes over time. The Guyatt's responsiveness index for the ADL subscale and the Sport subscale was respectively 2.75 and 1.40. The sport subscale of the FAAM seems to be less responsive than the ADL subscale. The minimal detectable change (MDC) based on a 95% confidence interval was 5.7 and 12.3 points for the ADL and Sports subscales, respectively.<ref name="4" /> | As well the ADL subscale as the Sport subscale of the FAAM were sensitive to significant changes over time. The Guyatt's responsiveness index for the ADL subscale and the Sport subscale was respectively 2.75 and 1.40. The sport subscale of the FAAM seems to be less responsive than the ADL subscale. The minimal detectable change (MDC) based on a 95% confidence interval was 5.7 and 12.3 points for the ADL and Sports subscales, respectively.<ref name="4" /> | ||
Significantly different change in scores during 4 week in the group expected to change (P<0.001).<ref name="6" /> | Significantly different change in scores during 4 week in the group expected to change (P<0.001).<ref name="6" /> | ||
== Links == | == Links == | ||
| Line 66: | Line 67: | ||
<references /> | <references /> | ||
[[Category:Outcome_Measures]] [[Category:Ankle]] [[Category:Foot]] [[Category:Musculoskeletal/Orthopaedics]] [[Category:Vrije_Universiteit_Brussel_Project]] | [[Category:Foot and Ankle Examination]] [[Category:Outcome_Measures]] [[Category:Ankle]] [[Category:Foot]] [[Category:Musculoskeletal/Orthopaedics]] [[Category:Vrije_Universiteit_Brussel_Project]] | ||
Revision as of 19:08, 10 March 2017
Original Editors - Niels Verbeeck
Top Contributors - Niels Verbeeck, Jeroen Van Cutsem, Admin, Evan Thomas, Kim Jackson, Wanda van Niekerk, WikiSysop, Mariam Hashem and Simisola Ajeyalemi
Intended PopulationCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
The Foot and Ankle Ability Measure (FAAM) is a self-report outcome instrument developed to assess physical function for individuals with foot and ankle related impairments. This self-report outcome instrument is available in English, German, French and Persian. The Foot and Ankle Ability Measure is a 29-item questionnaire divided into two subscales: the Foot and Ankle Ability Measure, 21-item Activities of Daily Living Subscale and the Foot and Ankle Ability Measure, 8-item Sports Subscale. The Sports subscale assesses more difficult tasks that are essential to sport, it is a population-specific subscale designed for athletes.
The FAAM is identical to the FADI, except for an additional 5 items found on the FADI. Four ‘pain related’ items of the Foot and Ankle Disability Index and the ability of an individual to sleep are deleted. The Sports subscale of the FAAM remains the same as the FADI Sports subscale.
Each item is scored on a 5-point Likert scale (4 to 0) from ‘no difficulty at all’ to ‘unable to do’. Item score totals, which range from 0 to 84 for the ADL subscale and 0 to 32 for the Sports subscale, were transformed to percentage scores. Higher scores represent higher levels of function for each subscale, with 100% representing no dysfunction.
Eechaute et al Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title(level 1) concluded that the FADI and FAAM were the most appropriate, patient-assessed instruments to quantify functional disabilities in patients with chronic ankle instability, but reported that there is need for further research of the FAAM in a specific population of patients with CAI.
Method of UseCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
The ADL and Sports subscales are scored separately.
The response to each item on the ADL subscale is scored from 4 to 0, with 4 being ‘no difficulty’ and 0 being ‘unable to do’. N/A responses are not counted. The score on each of the items are added together to get the item score total. The total number of items with a response is multiplied by 4 to get the highest potential score. If the subject answers all 21 items, the highest potential score is 84. If one item is not answered the highest score is 80, if two are not answered the total highest score is 76, etc. The item score total is divided by the highest potential score. This value is then multiplied by 100 to get a percentage. A higher score represents a higher level of physical function.
The Sports subscale is scored the same as above, 4 being ‘no difficulty at all’ to 0 being ‘unable to do’. The score on each item are added together to get the item score total. The number of items with a response is multiplied by 4 to get the highest potential score. If the subject answers all 8 items the highest potential score is 32, if one item is not answered the highest potential score is 28, if two are not answered the highest potential score is 24, ect. The item score total is divided by the highest potential score. This value is multiplied by 100 to get a percentage. A higher score represents a higher level of physical function.
For the most valid results it is suggested that scores for the FAAM ADL and Sports subscales be generated only when subjects completed 90% or more of the items (19 of 21 for the ADL and 7 of 8 for the Sports subscales respectively).
Evidence[edit | edit source]
 [edit | edit source]
[edit | edit source]
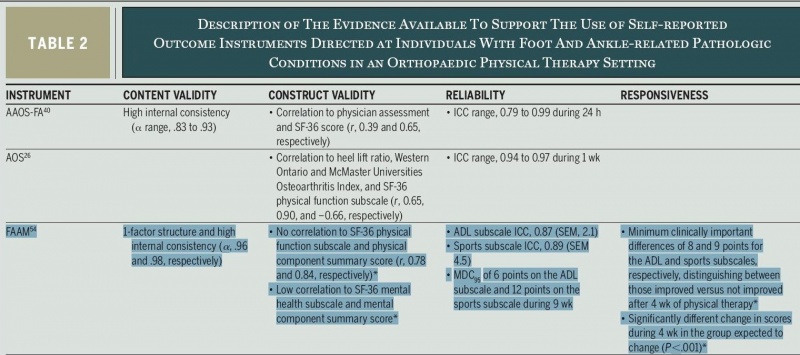
Evidence for content validity, construct validity, reliability, and responsiveness was obtained among 243 subjects who were separated into a group expected to change and a group expected to remain stable.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Reliability[edit | edit source]
The stability of a score with repeated measurements over time is defined as test-retest reliability. It is assessed by having an individual complete the instrument 2 or more times during a period when the individual’s condition is expected to remain stable. Intraclass correlation coefficient and SEM values are commonly used to estimate test-retest reliability.
Evidence for reliability was obtained using the group that was expected to remain stable.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- ADL subscale: ICC = 0.89; SEM = 2,1 points
- Sport subscale: ICC = 0.87; SEM = 4,5 points
Validity
[edit | edit source]
Content validity
The specific items on the instrument and what they measure determine the evidence that is based on content. The International Classification of Functioning, Disability and Health model can be used to define item content. According to this model, items can potentially measure the domains of (1) body structure and function and (2) activity and participation.'Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
For the development of the FAAM, the refined version of the FADI, both experts and patients were involved in the final item reduction. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Construct validity
While evidence for content relates directly to what the items measure, evidence for construct validity assesses how the scores on the instrument relate to other measures of the construct.60 A strong relationship between the scores on the instrument and other measures of the same or a related construct provides evidence for convergent validity; little or no relationship between the scores on the instrument and other measures of distinctly different constructs provides evi¬dence for divergent validity.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The ADL and Sport subscales of the FAAM were correlated to the SF-36 physical function subscale and the SF-36 mental function subscale. Strong correlations were found with the SF-36 physical function subscale (r = .84; r = .78), weak correlations were found with the SF-36 mental function subscale (r = .18; r = .11).Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- RobRoy L. Martin Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title(level 2) found evidence of validity for the FAAM ADL subscale as an outcome instrument to measure physical function in individuals with diabetes and foot and/or ankle related disorders, but further research is needed for the Sports subscale in individuals with diabetes. - Christopher R. Carcia et al Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title(level 3) study provides evidence of construct validity for the FAAM. The FAAM may be used to detect self-reported functional deficits in athletes related to Chronic Ankle Instability. Further research is needed.
- Thomas G. Mcpoil et al Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title says clinicians should use validated self-report questionnaires, such as the Foot Function Index (FFI), Foot Health Status Questionnaire (FHSQ), or the Foot and Ankle Ability Measure (FAAM) to measure physical function in individuals with heel pain/plantar fasciitis. Only the FAAM has been validated in a physical therapy practice setting. - Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title The FAAM may be used to collect data from all subjects with foot and ankle disorders such as rheumatoid arthritis, osteoarthritis, ankle sprains and ankle fractures.
Responsiveness
[edit | edit source]
Evidence for responsiveness assesses the ability of the instrument to detect changes in an individual’s status over time. The score on an outcome instrument should increase and decrease if the individual’s condition improves and worsens, respectively.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
As well the ADL subscale as the Sport subscale of the FAAM were sensitive to significant changes over time. The Guyatt's responsiveness index for the ADL subscale and the Sport subscale was respectively 2.75 and 1.40. The sport subscale of the FAAM seems to be less responsive than the ADL subscale. The minimal detectable change (MDC) based on a 95% confidence interval was 5.7 and 12.3 points for the ADL and Sports subscales, respectively.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Significantly different change in scores during 4 week in the group expected to change (P<0.001).Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Links[edit | edit source]
- FAAM (MS Word format)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1hgsEQZ6hYlnDg_C40T58HtQMzlZAAaBPz3bQtmetBWPwDD9g_|charset=UTF-8|short|max=10: Error parsing XML for RSS






