Baker's Cyst
Original Editor - Agapi Hakobyan
Top Contributors - Claudia Karina, Admin, Sheik Abdul Khadir, Chenoa Morales Caceres, Laura Ritchie, Kaviesha Madurapperuma, Agapi Hakobyan, Kim Jackson, Candace Goh, WikiSysop, Evan Thomas and Scott Buxton
Search strategy[edit | edit source]
We started our project regarding the Baker’s cyst by looking for information in pubmed and web of science. Our search terms included “Baker’s cyst” or “Popliteal cyst” and furthermore “clinical presentation”, “treatment”, “physical therapy”. We also looked for as many as possible other physio-pedia pages. To illustrate things better we also used youtube.
Definition/Description[edit | edit source]
| [1] |
A popliteal cyst, better known as a Baker’s cyst Baker's cyst, popliteal cyst, is a swelling filled with fluid that is located in the popliteal fossa region . (10) because it can be found incidentally during examination of the knee. It is called so after Dr. William Baker who first described this condition in 1877. Ganglia which are benign cystic tumors, originate from synovial tissue. It can occur mostly at the wrist, hand, foot, and knee which is known as popliteal cyst[2][3]. The most common occurrence of a Baker’s cyst is a distension of the bursa, located between the gastrocnemius and semimembranosus tendons . (8)(10)
The fluid finds its way through the channel the normal bursa communicate with the joint or by forming a hernia of the synovial membrane. (8)
The cyst can exercise pressure on some anatomical structures, in most cases, the affected anatomical structure is the popliteal vein. Which can develop into a thrombophlebitis. (8)
There are differences between a popliteal cyst in children and in adults. Popliteal cysts (Baker cyst) are commonly seen in children and are different than in adults. In children, there are cystic masses filled with gelatinous material that develop in the popliteal fossa, are usually asymptomatic, and are not related to intra-articular pathology. Spontaneous resolution usually occurs, although the process can take several years. In adults, a Baker’s cyst is often found in combination with other intra-articular pathologies and inflammatory conditions (meniscal tears, infectious arthritis,…). (9) (10)
Clinically Relevant Anatomy[edit | edit source]
A Baker’s cyst is an enlarged bursa that is normally located between the medial head of the gastrocnemius and a capsular reflection of the semimembranousus, named oblique popliteal ligament.
The two requirements for a cyst formation are the anatomical communication and a chronic effusion. Knee joint effusions may replete the gastrocnemius-semimembranosus bursa with synovial fluid and if the fluid outflow is hindered by a unidirectional mechanism, the gastrocnemius-semimembranosus bursa enlarges giving rise to a pseudocystic cavity, referred to as a Baker’s cyst[2].
Epidemiology /Etiology[edit | edit source]
A Baker’s cyst, or a popliteal cyst, occurs if there is an underlying problem with the knee.
The cyst can be split in an primary and secondary cyst. We speak of a primary cyst when there is an expansion arising independently from the joint and there is no knee derangement. The cyst is called a secondary cyst when there is a contact between the bursa and the knee joint. The cyst can be filled with fluid and a pathologic proces that may extend to the bursa. Most cysts are secondary cysts.
Popliteal cysts rarely come alone, they usually co-occur with other different intra -articular pathologies and inflammatory reactions. Baker’s cysts occur often secondary to other intra-articular pathologies, such as osteoarthritis, rheumatoid arthritis, meniscus pathology, effusion, ACL tears, knee pain and other pathologies[2].
Symptoms can include
• pain,(2)
• swelling and a mass(2)
• stiffness sometimes increased by activity (8) (9)
• tightness behind the knee.(2)
• Vague posterior knee pain(8) (9)
The cyst can vary in size, from a very small cyst to a large one. Smaller cysts may be asymptomatic, but a change in size is very common. Especially in smaller cysts, a septum may exist separating the semimembranosus and gastrocnemius components. This may function as a flap valve allowing fluid to enter a popliteal cyst and not to exit it. Cysts may range in size from small, from clinically not palpable to large masses causing visible swelling of the patient’s knee. If the cyst is large, it may result in mechanical problems in knee flexion and limiting mobility (2). Popliteal cysts can give pressure against other anatomic structures. Compression of the popliteal artery or vein can cause ischemia or thrombosis, respectively, whereas compression of the tibial or peroneal nerve can cause peripheral neuropathy.
The treatment for popliteal cysts can be performed in different ways. Sometimes no treatment or simple supportive measures lead to spontaneous resulation or to a reduction of the symptoms. If this does not happen, invasive and surgical techniques may be an option. (8) (9)
clinical presentation[edit | edit source]
Typical symptoms for a Baker’s cyst are vague posterior knee pain, a mass in the popliteal space and tightness in the back of the knee. A ruptured cyst can manifest as calf pain or even swelling, it can also cause an itching feeling in the calf. Ruptured cysts are more common in patients with an inflammatory pathology, than in patients with a degenerative pathology. (8)
Patients with a Baker’s cyst may have a limited range of motion. Most cysts are found on the medial side of the popliteal space in the gastrocnemius-semimembranosus bursa, but in some cases the cyst is in the popliteal bursa, and the mass will be found on the lateral side of the popliteal space. In examination, a cyst may not always be felt, however, this does not mean that it is not there. One test for finding a Baker’s cyst is the Foucher sign, which is further explained in the examination. (9)
Differential Diagnosis[edit | edit source]
Baker’s cyst can be mistaken for several other injuries in the knee. The patient’s history, as well as the clinical investigation and imaging allow for proper differential diagnosis of the disease.
Lipoma -> less resisting pressure, when compared to a Baker’s cyst
Aneurysm -> differentiated by Doppler evaluation (ultrasound)
Muscular herniation -> rare, history of a traumatic incident
Bursae of the biceps tendon, the semitendinosus tendon or pes anserinus tendons -> located medial and lateral to the knee joint. There is no inflammatory background or a history of internal derangement.
Differentiation from thrombophlebitic symptoms is difficult because the baker’s cyst itself appears to be at the base of vascular obstructive symptoms in the calf. Precise differentiation of the patient’s symptoms can be located by ultrasonography. (8) (11)
If the popliteal cyst becomes infected, this can often result in a painful mass behind the knee. In such cases, it could be difficult to make a diagnosis and the infected cyst can be mistaken for a neoplasm. The cyst can rupture (split open) resulting in severe calf pain, decreased motion at the ankle and cause similar symptoms as a deep vein thrombosis (evident on ultrasound or venogram).
It is important to diagnose a ruptured Baker’s cyst early and to differentiate it from
• thrombophlebitis
• popliteal aneurysm
• inflammatory arthritis
• medial gastrocnemius strain
• soft-tissue tumor or muscle tear
in order to determine the best treatment and avoid complications, such as compartment syndrome.(4)
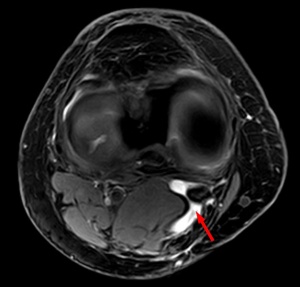
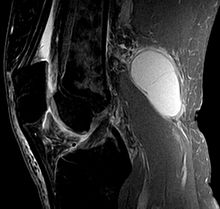
Diagnostic Procedures[edit | edit source]
The imaging workup of knees with suspected popliteal cysts can include plain radiographs, arthrography, ultrasound, and MRI. Early in the evaluation it can be useful to obtain plain radiographs (as posteroanterior Rosenberg, lateral, and patellofemoral axial views) for detecting other conditions found in association with popliteal cysts, such as osteoarthritis, inflammatory arthritis and loose bodies. In addition, loose bodies may be seen in a Baker’s cyst on plain radiographs.
At first, direct arthrography was used for detecting popliteal cysts. Direct arthrography involved intra-articular injection of the knee with gas or an iodinated contrast medium, followed by mobilization of the joint to force the contrast into the cyst. Afterwards spot radiographs or fluoroscopy were used to detect the presence of the contrast in the cysts. Disadventages of this technique include the use of ionizing radiation and the use of invasive techniques to inject the contrast.
The advantages of ultrasound provide a replacement of arthrography by ultrasound. The advantages are its low cost, noninvasive usage and the absence of radiation. The main disadvantage is the fact that it is user dependent. Ultrasound is able to detect Baker’s cysts near 100%, but lacks to differentiatie from other conditions, such as meniscal cysts or myxoid tumors, it also doesn’t visualize other conditons in the knee that are often associated with these cysts.
The gold standard for diagnosis of Baker’s cysts and differentiating them from other conditions remains magnetic resonance imaging. It allows assessment of the entire spectrum of related disorders. Conditions such as meniscal cysts are more easily differentiated from Baker’s cysts with MRI than ultrasound. This may be the gold standard but is also a high cost technique, therefore, ultrasound should be considered as a sreening modality if evaluation of the intra-articular structures is not necessary. (12)
The size of the cyst or pain can cause limitations in range of motion. In rare cases there will be signs and symptoms of a meniscal tear which can be tested by McMurray test[2].
Outcome measures[edit | edit source]
Outcome measures used to determine and evaluate the expected results of the therapy/procedure to be compared to the results found within the patient.
• Western Ontario and McCaster universities pain subscale(WOMAC): Is an multidimensional instrument that measures 17 functional activities , 5 pain-related activities and joint stiffness categories. It measures pain and dysfunction
• Visual analog scale(vas):
It measures pain on a line from 0 to 10. From no pain to extreme pain. It is easy or the patient to mark how much pain he/she has.
• The Rauschning and Lindgren classification(RL): was used to evaluate the outcome and therapeutic efficacy. Grading is from 0 to 3
• The Newcastle-ottowa scale(NOS): Is a simple scale to evaluate the quality of non-randomized controlled studies (13) (14) (15)
Examination
[edit | edit source]
Patients with a Baker’s cyst commonly have symptoms of meniscal or chondral pathology. Symptoms related to a popliteal cyst are rare. If these symptoms are present, they may be related to the size of the cyst. Symptoms related to the cysts include posterior or posteromedial fullness and achiness, mass and stiffness. The most common symptoms are popliteal swelling and posterior aching. Patients may also complain of pain that occurs with terminal knee extension. (12)
During the examination testing of knee flexion can be usefull. Patients with large cysts may develop loss of knee flexion because the cysts mechanically block flexion. Examination will often reveal knee meniscal or chondral pathology. If the cyst is large, there can be palpable posteromedial fulness or tenderness. A palpable cyst is often firm in full knee extenstion and soft in knee flexion. This finding is known as “foucher sign” and is due to cyst compression. With extension the gastrocnemius and the semimembranosus muscles approximate each other and the joint capsule compressing the cyst against the deep fascia. The mechanism of Foucher’s sign is usefull for distinguishing Baker’s cysts from lesions such as popliteal artery aneurysms, adventitial cysts, ganglia and sacromas, for which the palpation of the mass is unaffected by the knee postion. (16)
The size of the cyst or pain can cause limitations in range of motion. In rare cases there will be signs and symptoms of a meniscal tear which can be tested by McMurray test[4].
Medical Management[edit | edit source]
By a popliteal cyst of inflammatory origin it is enough to treat the underlying disease. When the underlying disease doesn’t get treated, the Baker’s cyst can come back. Arthroscopic examination should be performed and all pathologic conditions treated before considering the excision of a popliteal cyst. (8) [l.O.E. 5]
The asymptomatic popliteal cyst often gets better and disappears by itself over time. The cyst can be removed with surgery if it becomes very large or causes symptoms such as discomfort, stiffness or painful swelling.(4) [L.O.E. 2A] (11) [L.O.E. 2A]
There are three surgical techniques available to treat the cyst: common posterior approach, the posteromedial approach and the medial intra-articular approach. The first two techniques are techniques where the cyst is going to be removed. In the last technique they make an opening in the cyst and close it afterwards. The popliteal cyst will eventually disappear. (8) [L.O.E. 5]
Rest can temper the pain that bursa is causing. Treatment of Baker’s cyst consists taking non-steroidal anti-inflammatory drugs (NSAID) to alleviate the pain, restrict movement, alternate ice.
If the pain persist, an subsequent steroid injection with a solution of anaesthetic and steroid can be advised which can relieve pain, but not prevent recurrence of the cyst. It’s only a temporary solution. (8) [L.O.E. 5]
Physical Therapy Management[edit | edit source]
An ice massage of 15 minutes every 4-7 hours will reduce the inflammation. The treatment is based on the principles of R.I.C.E (rest, ice, compression, and elevation) followed by some muscle-conditioning exercises.
Rehabilitation program can improve the control of the knee joint by range of motion exercises. It will increase the motion of the joint as well as increase flexibility. The physiotherapist will give a mobility, a hamstring stretching program and a concurrent quadriceps strengthening program that has to repeated several times a day. This will result in less pain at about 6-8 weeks.
We have found an experiment comparing ultrasound guided corticosteroid injections with a horizontal therapy. 60 people were divided in three groups, only injections (group A), only horizontal therapy (group B) and (group C) they got both the injections and the horizontal therapy. The horizontal therapy was delivered through a specific commercial device, and they followed the instructions, provided by the manufacturer. Patients in groups A and C had a lower level of pain after one month. Group C had the lowest VAS scores and group C also scored best on the WOMAC. In group B and C the stiffness and disability scores were also improved the most. (13) [L.O.E. 1B]
| [3] | [4] |
Key research[edit | edit source]
Daniel F. et al. The popliteal cyst. Knee surg sports traumatol arthrose 2006 14:623-628(8)
Alysa M. Popliteal cystc: a current review. Healio.com/orthopedics 2014 vol 37 number 8 pages 678-684(9)
Resources[edit | edit source]
Jin Hwan Ahn, M.D., Sang Hak Lee, M.D., Jae Chul Yoo, M.D., Moon Jong Chang, M.D., and Yong Serk Park, M.D. Arthroscopic Treatment of Popliteal Cysts: Clinical and Magnetic Resonance Imaging Results. Original Article With Video Illustration. 2010 Oct;26(10):1340-7. Epub 2010 Sep 24. Quality level C1(therapeutically series)
For finding answers to the problem of a popliteal cyst we used different resources, such as pubmed, web of science and google scholar. We also found out that there is not much research in the physical therapy treatment, more research exists on the surgical treatment. We think that there is more that physical therapists could do, if there was more research.
Clinical bottom line[edit | edit source]
Baker’s cysts have different causes, therefore finding one solution is difficult. The most common treatments are invasive, such as corticosteroid injections and NSAID or surgery. When the pain is worse, an injection can help to relieve the pain. However, it cannot ensure that the cyst will not come back. In the different examinations, we have found that often the cyst disappears by itself. However, this is not always the case. A patient who has a lot of pain from the Baker’s cyst may use ice or NSAID, in order to reduce the pain. At this stage, there is a need for more research on physical therapy, applied on Baker’s cyst patients.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1b_xvYg: Error parsing XML for RSS
Read 4 Credit[edit | edit source]
|
Would you like to earn certification to prove your knowledge on this topic? All you need to do is pass the quiz relating to this page in the Physiopedia member area. |
References[edit | edit source]
1. ↑ nabil ebraheim. Baker's Cyst - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: http://www.youtube.com/watch?v=kH6of0ipfXw [last accessed 12/09/14]
2. ↑ 2.0 2.1 2.2 Peter Larking. Causation Review – Popliteal Cysts/Baker’s Cyst of the knee. Governance, Policy and Research, ACC, 03- 2011. Quality level A2 (causation review)
3. ↑ Walter B. Greene, MD - editor. 2nd edition. USA(2001). Essentials of Muscluloskeletal Care. Section 6, Knee and Lower leg - popliteal cyst (p.397-398)fckLRQuality level D (opinion of experts)
4. ↑ 4.0 4.1 4.2 WC Torreggiani, K Al-Ismail, PL Munk, C Roche, C Keogh, S Nicolaou, LP Marchinkow. The imaging spectrum of Baker's (Popliteal) cysts. Clinical Radiology. 2002 Aug;57(8):681-91. Quality level A2 (review)
5. ↑ Calvisi, Vittorio, Lupparelli, Stefano, Giuliani, Pierandrea. Arthroscopic all-inside suture of symptomatic Baker's cysts: a technical option for surgical treatment in adults. Knee Surgery Sports Traumatology Arthroscopy. 2007 Dec;15(12):1452-60. Epub 2007 Aug 1. Quality level C3 (not strong evidence)
6. ↑ Westside-Medical. Baker's Cyst Treatment Feat. Dr. Blake Staker Westside-Medical. Available from: http://www.youtube.com/watch?v=xjX9jBWXLkM [last accessed 12/09/14]
7. ↑ TheGVideo. Massaging bakers cyst. Available from: http://www.youtube.com/watch?v=ETorNuyS4JA [last accessed 12/09/14]
8, Daniel F. et al. The popliteal cyst. Knee surg sports traumatol arthrose 2006 14:623-628 (level 5 expert opnion)
9,Alysa M. Popliteal cystc: a current review. Healio.com/orthopedics 2014 vol 37 number 8 pages 678-684. Quality level 2A (review)
10, Di Sante, Luca, et al. "Ultrasound-guided aspiration and corticosteroid injection of Baker's cysts in knee osteoarthritis: a prospective observational study." American Journal of Physical Medicine & Rehabilitation 89.12 (2010): 970-975. Quality level 1B (RCT)
11, Handy, John R. "Popliteal cysts in adults: a review." Seminars in arthritis and rheumatism. Vol. 31. No. 2. WB Saunders, 2001. Quality level 2A (review)
12. Frush, Todd J., and Frank R. Noyes. "Baker’s Cyst Diagnostic and Surgical Considerations." Sports Health: A Multidisciplinary Approach 7.4 (2015): 359-365.) level 4
13. L. DI Sante; Ultrasound-guided aspiration and corticosteroid injection compared to horizontal therapy for treetment of knee osteoarthritis complicated with Baker’s cyst: a randomized controlled trial; European journal of physical and rehabilitation medicine; 2012 vol. 48 level 1b
14. Xiao-nan Zhou, Bin Li, Jia-shi Wang and Lun-hao Bai*, Surgical treatment of popliteal cyst: a systematic review and meta-analysis, Zhou et al. Journal of Orthopaedic Surgery and Research (2016) 11:22 level 1a
15. Francesca Bandinelli, Roberto Fedi, Sergio Generini, Francesco Porta, Antonio Candelieri ,Alessandro Mannoni, Massimo Innocenti, Marco Matucci Cerinic, Longitudinal ultrasound and clinical follow-up of Baker’s cysts injection with steroids in knee osteoarthritis, April 2012, Volume 31, Issue 4, pp 727–731level 2b
16. (Canoso, J. J., et al. "Foucher's sign of the Baker's cyst." Annals of the rheumatic diseases 46.3 (1987): 228-232.) level
- ↑ nabil ebraheim. Baker's Cyst - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: http://www.youtube.com/watch?v=kH6of0ipfXw [last accessed 12/09/14]
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedTorreggiani - ↑ Westside-Medical. Baker's Cyst Treatment Feat. Dr. Blake Staker Westside-Medical. Available from: http://www.youtube.com/watch?v=xjX9jBWXLkM [last accessed 12/09/14]
- ↑ TheGVideo. Massaging bakers cyst. Available from: http://www.youtube.com/watch?v=ETorNuyS4JA [last accessed 12/09/14]