Axillary Nerve Injury
Original Editor - Kimberley Anlauf
Top Contributors - Kimberley Anlauf, Vidya Acharya, Kim Jackson, Amanda Ager, Garima Gedamkar, Samuel Adedigba, Uchechukwu Chukwuemeka, Bianca Camacho, Evan Thomas, 127.0.0.1, Admin, Johnathan Fahrner, WikiSysop, Tony Lowe, Leana Louw, Michael Gillespie, Chrysolite Jyothi Kommu, Wendy Walker, Naomi O'Reilly, Claire Knott, Jose Antonio Cadena, Abbey Wright, Jeremy Brady and Peter Zatezalo
Definition/Description[edit | edit source]
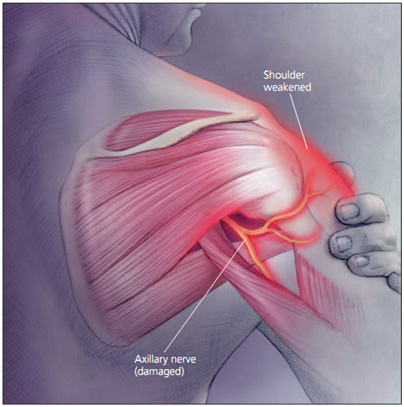
It is characterized by trauma to the axillary nerve from either a compressive force or traction injury following anterior dislocation of the shoulder.[1][2][3][4][5][6][7][8][9][10]
Axillary nerve injury is also called neuropathy of the axillary nerve. It describes a loss of movement or lack of sensation in the shoulder area of the body. Stress or damage to the axillary nerve, which serves the deltoid muscles and skin of the shoulder, causes this dysfunction.
Since this is a problem with just one nerve, it is a type of Peripheral neuropathy called mononeuropathy. Of all brachial plexus injuries, axillary nerve palsy represents only .3% to 6% of them
Epidemiology/Etiology[1][2][3][4][5][6][7][8][9][10][edit | edit source]
- Anterior shoulder dislocation is the most common occurring dislocation at the shoulder.[2][3][4][5][6][8][9]
- Men and women 3:1[5]
- 9-65% involve axillary nerve injury[2][8][9][11][12]
- 23% have combination neuropathies, all involving the axillary nerve[8]
- The incidence of brachial plexus and axillary nerve injury increases dramatically following shoulder dislocation in patients ≥50 years of age, if fracture is associated with the dislocation, and if the duration of the dislocation lasts >12 hours[8][9][10][13][14]
- Incidence of nerve injury doubled with the presence of an associated fracture[10]
- Incidence of nerve injury doubled with the presence of an associated fracture[10]
- Traction and compression to the axillary nerve[1][2][6][7][9][10][2]
- The axillary nerve becomes stretched across the humerus as it dislocates anteriorly and inferiorly.[2][9]
- Propagated tension due to overstretching of the axillary nerve over the humeral head during shoulder dislocations may cause elongation of the free portion of the axillary nerve and the increased tension may even result in axillary nerve avulsions from the posterior cord of brachial plexus.[2][9]
- The axillary nerve is susceptible to injury at several sites, including the origin of the nerve from the posterior cord, the anterior inferior aspect of the subscapularis muscle and shouler capsule, the quadrilateral space, and within the subfascial surface of the deltoid muscle.[9]
- The axillary nerve becomes stretched across the humerus as it dislocates anteriorly and inferiorly.[2][9]
- Nerve Injury Overview
- Nerve regeneration takes place at a rate of ~1mm/day
- Seddon's Classification of Nerve Injury
- Neuropraxia
- The axon and all 3 connective tissue layers (endoneurium, perineurium, and epineurium) remain intact with a decrease in conduction
- Comparable to a 1st degree nerve injury (Sunderland's Classification of Nerve Injury)
- The axon and all 3 connective tissue layers (endoneurium, perineurium, and epineurium) remain intact with a decrease in conduction
- Axonotmesis
- Axonal damage is present with preservation of the endoneurium
- The endoneurium acts as a guide for axonal regeneration
- Comparable to a 2nd degree degree nerve injury
- Axonal damage is present with preservation of the endoneurium
- Neurotmesis
- Axonal damage is present
- Connective sheath damage ranges from partial disruption of the endoneurium to complete disruption of the involved nerve
- 3rd degree nerve injury= axon and endoneurium are damaged with preservation of the perineurium
- 4th degree nerve injury= axon, endoneurium, and perimeurium are damaged with presercation of the epineurium
- 5th degree nerve injury= complete disruption of the nerve
- Neuropraxia
Characteristics/Clinical Presentation[edit | edit source]
It is important to note that the clinical presentation of axillary nerve dysfunction is variable and can go undetected, as the concomitant dislocation or fracture may mask the symptoms.[1][9] Nerve injury should be considered as part of the differential diagnosis process when a patient reports pain, weakness, or paresthesias.[7]
- Subjective Examination
- Generalized mild, dull, and achy pain to the deep or lateral shoulder, with occasional radiation to the proximal arm [4][6][15][16]
- Numbness and tingling of the lateral arm and/or posterior aspect of the shoulder [4][6][7][9][14][16]
- In some cases, persisting 2-4 weeks post-injury
- In some cases, persisting 2-4 weeks post-injury
- Feeling of instability[16]
- Weakness, especially with flexion, abduction, and external rotation [6][9][15][16]
- Fatigue, especially with overhead activities, heavy lifting, and/or throwing [7][14][15]
- May/or may not reveal a history of trauma to the shoulder region [4][6]
- History of dislocation with soreness persisting ~1week post-injury [16]
- Easing Factors include: rest, ice, analgesics, and anti-inflammatory medications [6][7][17]
- Generalized mild, dull, and achy pain to the deep or lateral shoulder, with occasional radiation to the proximal arm [4][6][15][16]
Many athletes with axillary nerve injury may be asymptomatic with incomplete or complete lesions, with the only complaints of weakness and early-onset fatigue with exercise. [4][14]
Differential Diagnosis[edit | edit source]
Axillary nerve injury with shoulder dislocation can present similarly to or concomitantly with the following conditions: [9][13][15]
- “Unhappy Triad”
- Quadrilateral Space Syndrome (QSS)
- Posterior Cord of the Brachial Plexus Injury
- C5-6 Cervical Radiculopathy
- Parsonage-Turner Syndrome (PTS)
"Unhappy Triad"
The “Unhappy Triad” consists of a shoulder dislocation that results in both a rotator cuff tear and axillary nerve injury.
- Occurs in 9-18% of anterior shoulder dislocations[8]
- Risk of an “unhappy triad” with anterior shoulder dislocation increases after the age of 40[8]
Quadrilateral space syndrome(QSS)
QSS is an “uncommon condition that involves the compression of the posterior humeral circumflex artery and the axillary nerve within the quadrilateral space,” secondary to an acute trauma or from overuse, especially with overhead sports like throwing and swimming.[17]
- 4 Cardinal Features[17]
- Generalized shoulder pain
- Paresthesias in a nondermatomal pattern
- Point tenderness to the quadrilateral space
- (+) arteriogram findings with the shoulder in abduction and external rotation
- Symptoms are typically present with the arm in an overhead position, especially in late cocking or the early acceleration phases of throwing[17]
Parsonage-Turner Syndrome(PTS)
PTS is an uncommon, idiopathic condition, characterized by an acute onset of intense pain, without a mechanism of injury, that subsides within days-weeks, leaving behind residual weakness/paralysis in upper extremity muscles.[18]
- Symptoms are NOT related to neck movements.
- Aka: Acute brachial neuritis
For more details, see Differential Diagnosis Chart.[6][7][8][9][13][14][15][16][17][18][19][20][21]
Examination[edit | edit source]
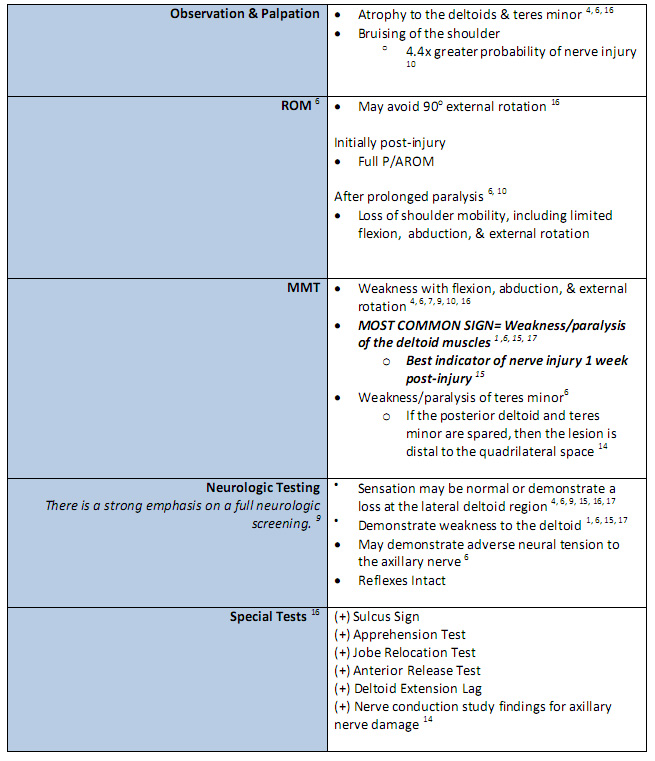
Physical examination should begin with a screening consisting of an evaluation of the head and neck which shouldn’t reveal any abnormalities.[9][16] If the patient presents with a recent shoulder dislocation, presence of a radial pulse and sensation and movement of the digits should also be assessed as part of the initial screening.[7]
Figure 3[1][4][6][7][9][10][14][15][16][17]
| [22] | [23] |
Click for more information on the Sulcus Sign Click for more information on the Apprehension & Jobe Relocation Test
It is important to note that the physical examination findings are dependent on the extent of the axillary nerve damage. Furthermore, there is a lack of consensus regarding the ability of a patient to retain normal range of motion and function when presenting with axillary nerve injury. [9]
Image:Axillary_Nerve_Injury_Fig_6.jpgFigure 6 [9][14][17]
Accurate manual muscle testing is necessary as 60% of athletes may be able to elevate the effected arm by compensating with and recruiting the pectoralis major and supraspinatus muscle groups, and prevent subluxation by utilizing the supraspinatus and long head of the biceps muscles. [4][9][14] However, there is no evidence to translate this statistic to the general population.
The sensory examination of the axillary nerve has been calculated to have a poor sensitivity (7%) in detecting the presence of axillary nerve injury, emphasizing the need for electrodiagnostic evaluation for a patient with persistent weakness and decreased shoulder function following shoulder dislocation. [8][10]
Clinical Diagnosis[edit | edit source]
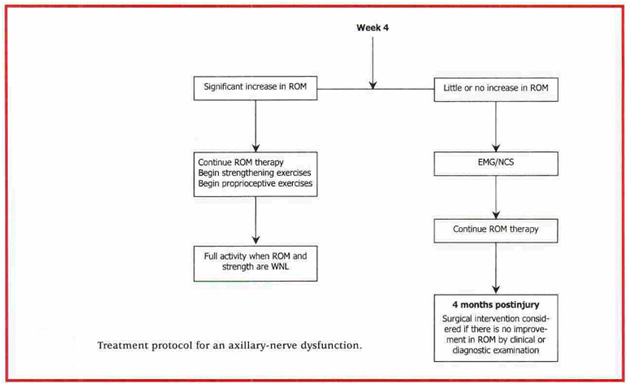
The best means to confirm a concomitant axillary nerve injury with shoulder dislocation includes detailed subjective and objective clinical examinations, along with EMG studies.[6]
- Clinical Exam
- EMG
- The diagnostic test of choice to identify nerve conduction loss is EMG
- EMG can distinguish between atrophy secondary to pain or that of nerve injury.[4]
- EMG studies also serves as means to track the patient’s progression or regression throughout the recovery phase, ultimately indicating whether a surgical or conservative treatment approach is needed
- MRI[7]
- MRI is rarely used for initial evaluation of a typical nerve injury
- It may be useful if the diagnosis is unclear or if there is evidence of abnormal recovery
- A normal MRI does not rule out nerve injury.
Prognosis[4][9][10][14][15][edit | edit source]
The duration of recovery from axillary nerve injury is prolonged, lasting as long as up to 35 weeks.[10]
- Excellent [4][9][15]
- Good [4][9]
- Axonotmesis (2nd degree) nerve injury
- The recovery rate is near 80% secondary to the short distance between the site of injury and the muscle endplates. [4][9]
- Recovery should be evident between 3-4 months post-injury [4]
- EMG re-evaluations should be preformed at monthly intervals for signs of regeneration.
- By 6 months post-injury, if there are no signs of functional return, surgical exploration and possible nerve grafting are recommended. [4]
- Poor[4][9]
- Neurotmesis (3rd-5th degree) nerve injury
- Without surgical intervention, there is typically no recovery. [9]
Medical Management (current best evidence)[edit | edit source]
Surgery[edit | edit source]
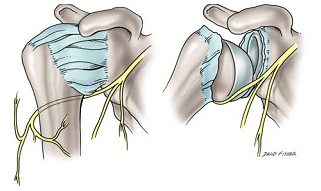
- “There is uncertainty among clinicians as to the appropriate time for surgical exploration following isolated axillary nerve injury, with some authors recommending exploration at 3 months post-injury while others recommend at 6 to 12 months post-injury.”[9][17] The site of the axillary nerve injury is variable, making both anterior and/or posterior surgical approaches appropriate.[4] If the axillary nerve cannot be repaired without tension, cable grafts are required. Indications for surgery are rare, but must be understood by clinicians in order to maximize outcomes and minimize complications.[7]
- Indications for surgery
- Surgery for shoulder instability in young active patients reduces the likelihood of recurrent anterior shoulder dislocations, therefore reducing the possibility of axillary nerve compromise.[24]
- In the rare occasion that surgery is indicated, there are several types of surgeries which can be considered by the patient and his surgeon.[7][14] There is a better prognosis if the surgery is performed within 6 months of the injury but functional improvements can be expected with surgical intervention up to 12 months year after the injury.[14][15] The clinician should be aware of these prognostic correlations between time of injury and time of surgery to maximize the patients outcome.
- Prognosis is good in 90% of patients [4]
- Surgical Procedures
Nonsurgical Reduction[edit | edit source]
- Reduction eliminates the need for surgical intervention, and is followed by immobilization and physical therapy management. [25]
- Precaution should be taken during manipulative reduction of a dislocation, in which traction together with rotation or abduction are applied simultaneously, creating extra distraction and increasing the risk of axillary nerve damage. [10]
- Other treatments include: NSAIDS, rest, ice [6][7][17][24]
Physical Therapy Management (current best evidence)[edit | edit source]
Current research encompassing treatment and intervention of axillary nerve injuries following shoulder dislocation is limited. The research suggests that the management of the axillary nerve damage following shoulder dislocation is treated in the same manner as treating an isolated dislocation, with an emphasis on strengthening and stimulation of the deltoids and teres minor muscles.[4][13] There should be a great amount of importance placed on allowing ligamentous, capsular, and nervous tissues time to heal while preventing joint stiffness, which could ultimately hinder function greater in the long run.[7][10][13]
Non-Surgical Physical Therapy Treatment[edit | edit source]
0-2 weeks[4][10][13][16][25][26]
- Shoulder immobilization via sling after reduction
- There is insufficient evidence to support whether physical therapy should be initiated during or after immobilization. [5]
- Isometric Strengthening; Dosing: 10 seconds X 6 repetitions X 2 day within limits of pain
- Shoulder(Flex, Ext, Abd, Add, IR)
- Joint Mobility
- Active Range of Motion(AROM); Dosing 10 repetitions X 2 day
- Elbow(Flex, Ext ,Pronation, Supination)
- Wrist (Flex, Ext, Radial/Ulnar deviation)
- Hand (Opening/Closing Fist)
- Active Range of Motion(AROM); Dosing 10 repetitions X 2 day
2-4 weeks
- Joint Mobility
- Passive/Active Assisted Range of Motion(PROM/AAROM); Dosing 10 repetitions X 2 day
- Shoulder (Flex, IR, Add)
- Avoid end-range ER/Abd until later stages of treatment!
- Shoulder (Flex, IR, Add)
- Active Range of Motion (AROM); Dosing 10 repetitions X 2 day
- Elbow(Flex, Ext ,Pronation, Supination)
- Wrist (Flex, Ext, Radial/Ulnar deviation)
- Hand (Opening/Closing Fist)
- Pendulum Exercises 3 sets x 30 seconds[13]
- Passive/Active Assisted Range of Motion(PROM/AAROM); Dosing 10 repetitions X 2 day
- Postural/Periscapular Muscular Strengthening/Neuromuscular Re-education[9][16][25]
Older individuals have lower rates of reoccurrence of shoulder dislocation and an increase in incidence of joint stiffness. Therefore, progressive strengthening and proprioceptive training should be initiated sooner than in younger individuals, who usually begin around week 6. [6][13]
4-6 weeks
- D/C sling
- Strengthening Program light resistive exercises [25]
- Target muscles
- Deltoids
- Rotator Cuff muscles
- Postural muscles
- Target muscles
- Proprioceptive Techniques [13][16][25]
- PNF diagonals
- Closed Chained Activities
- Wall push-ups -->Table-->Floor
- Weight Shifts
6 weeks-Discharge [3][24][27][28]
- Continue ROM, glenohumeral and scapulothoracic stabilization/strengthening exercises, proprioception, and joint mobility, while maintaining optimal conditions for tissue healing
- Begin to initiate sport/job specific activities, progressing to full return as patient’s functional status allows
There is no consensus of when return to sport/work is appropriate following an axillary nerve injury. In general, improvement on the EMG and at least 80% return of deltoid muscle strength is recommended. [3][24]
- It has been suggested that return to activity for shoulder dislocation is approximately 12 weeks, and 16 weeks for competitive sports. [27][28]
Note: Progression of these interventions with increased weight or resistance should be based on each individual patient and their level of pain and perceived joint stability throughout a controlled movement.[13]
Conservative physical therapy treatment can last between 3 to 6 months. It is essential that the physical therapist continuously monitor the progression of axillary nerve reinnervation during treatment and contact the patient’s physician if there are no signs of improvement between 3 to 4 months.[7][9]
For examples of therapuetic exercises, see Examples of TherEx in Axillary Nerve Injury Rehab.
Post-Surgical Physical Therapy[edit | edit source]
There is a lack of research to support how long a patient should be immobilized after surgical repair of the axillary nerve. Current recommendations report that the shoulder should be immobilized for 4 to 6 weeks, after which rehabilitation should focus on increasing shoulder range of motion and strengthening. [17]
Key Research[edit | edit source]
There is only minimal, low quality evidence regarding isolated axillary nerve injury in shoulder dislocations, consisting mostly of descriptive and exploratory studies.
- Nerve Injury About the Shoulder in Athletes, Part 1- A descriptive study that reviews the anatomy of the axillary nerve, presentation and clinical examination, diagnostic tests, differential diagnosis, and treatment of axillary nerve injury, with emphasis on early recognition and diagnosis of this type of injury.
- Axillary Nerve Injuries in Contact Sports: Recommendations for Treatment and Rehabilitation- A descriptive study that discusses the relevant anatomy, proper examination and diagnosis of the axillary nerve injury, differential diagnosis (to include cervical spine clearing), conservative treatment, indications for surgical intervention, complications and prognosis, and rehabilitation. In regards to treatment, there is emphasis placed on the axillary nerve injury in conjunction with the shoulder dislocation.
- The Effectiveness of Rehabilitation for Nonoperative Managment of Shoulder Instability: A Systematic Review- A systematic review of low level evidence regarding conservative managment for shoulder instability. Effective treatments found for patients with primary shoulder dislocation included 3-4 weeks immobilization, followed by 12 weeks of rehabilitation that included ROM and exercises that focused on stability directed towards the glenohumeral and scapularthoracic joints.
Resources
[edit | edit source]
CPR for Cervical Radiculopathy
Test Item Cluster- Full Thickness Rotator Cuff Tear
Medica: Professional Medical Search
Clinical Bottom Line[edit | edit source]
A standardized treatment is not yet known for patients with axillary nerve injury secondary to shoulder dislocation. However, immobilization based on age, treatments focused on ROM, strength, neuromuscular re-education, and function all seem to be a recurrent theme. With early detection, prognosis for the injured axillary nerve is good due to its short length needed to regenerate.
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Allen J, Dean K. Recognizing, managing, and testing an axillary- nerve dysfunction. Athletic Therapy Today. 2002;7(2):28-29.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Apaydin N, Tubbs S, Loukas M, Duparc F. Review of the surgical anatomy of the axillary nerve and the anatomic basis of its iatrogenic and traumatic injury. Springer. 2010;32:193-201.
- ↑ 3.0 3.1 3.2 3.3 3.4 Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl. 2009:91:2-7.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 Duralde X. Neurologic injuries in the athlete’s shoulder. Journal of Athletic Training. 2000;35(3):316-328.
- ↑ 5.0 5.1 5.2 5.3 5.4 Handoll HHG, Hanchard NCA, Goodchild LM, Feary J. Conservative management following closed reduction of traumatic ; anterior dislocation of the shoulder (review). Cochrane Database of Systematic Review. 2006;1:1-26.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 Miller T. Peripheral nerve injuries at the shoulder. The Journal of Manipulative Therapy. 1998;6(4)170-183.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 7.15 Neal S, Fields K. Peripheral nerve entrapment and injury in the upper extremity. American Family Physician. 2010; 81(2): 147-155.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 Payne M, Doherty T, Sequeira K, Miller T. Peripheral nerve injury associated with shoulder trauma: a retrospective study and review of literature. Journal of Clinical Neuromuscular Disease. 2002; 4(1): 1-6.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 9.14 9.15 9.16 9.17 9.18 9.19 9.20 9.21 9.22 9.23 9.24 9.25 9.26 9.27 9.28 9.29 9.30 9.31 Perlmutter G, Apruzzese W. Axillary nerve injuries in contact sports: recommendations for treatment and rehabilitation. Sports Med. 1998;26(5): 351-360.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 Visser C, Coene L, Brand R, Tavy D. The incidence of nerve injury in anterior dislocation of the shoulder and its influence on functional recovery a prospective clinical and emg study. Journal of Bone and Joint Surgery. British volume. 1999; 81-B(4). 679-685.
- ↑ Cox C, Kuhn J. Operatice versus nonoperative treatment of acute shoulder dislocation in the athlete. Current Sports Medicine Reports. 2008;7(5): 263-268.
- ↑ McFarland E, Caicedo J, Kim T, Banchasuek P. Axillary nerve injury in anterior shoulder reconstructions: use of a subscapularis muscle- splitting technique and a review of the literature. Am J Sports Med. 2002;30:601-606.
- ↑ 13.00 13.01 13.02 13.03 13.04 13.05 13.06 13.07 13.08 13.09 13.10 13.11 Kazemi M. Acute traumatic anterior glenohumeral dislocation complicated by axillary nerve damage: a case report. Journal of the Canadian Chiropractic Association. 1998;42(3):150-155.
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 14.12 Safran M. Nerve injury about the shoulder in athletes, Part 1: Suprascapular nerve and axillary nerve. Am J Sports Med . 2004;32(3):803-819.
- ↑ 15.00 15.01 15.02 15.03 15.04 15.05 15.06 15.07 15.08 15.09 15.10 15.11 15.12 Vitanzo P, Kenneally B. Diagnosis of isolated axillary neuropathy in athletes:case studies. The Journal of Musculoskeletal Medicine. 2009; 26:307-311.
- ↑ 16.00 16.01 16.02 16.03 16.04 16.05 16.06 16.07 16.08 16.09 16.10 Miller T. Axillary neuropathy following traumatic dislocation of the shoulder: a case study. The Journal of Manual & Manipulative Therapy. 1998;6(4):184-185.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 17.8 17.9 Manske R, Sumler A, Runge J. Quadrilateral space syndrome. Humen Kinetics-ATTI.2009;14(2):45-47.
- ↑ 18.0 18.1 Mamula C, Erhard R, Piva S. Cervical radiculopathy or parsonage-turner syndrome: differential diagnosis of a patient with neck and upper extremity symptoms. Journal of Orthopaedic Sports Physical Therapy. 2005; 55(10): 659-664.
- ↑ 19.0 19.1 Hertel R, Lambert SM, Ballmer FT. The deltoid extension lag sign for diagnosis and grading of axillary nerve palsy. J Shoulder & Elbow Surgery 1998;7(1):97-108.
- ↑ Wainner R, Fritz J, Irrgang J, Boninger M, Delitto A, Allison S. Reliability and diagnositic accuracy of the clinical examination and patient self report measures for cervical radiculopathy. SPINE. 2003; 28(1):52-62.
- ↑ Park H, Yokota A, Gill H, Rassi G, McFarland E. Diagnostic accuracy of clinical tests for the differential degrees of subacromial impingement syndrome. The Journal of Bone and Joint Surgery. 2005;87-A(7): 1446-1455.
- ↑ Chernchujit, B. Sulcus Sign Shoulder Dislocation Instability Examination [Video]. YouTube. http://www.youtube.com/watch?v=cTDoZo3HPz4. Published May 18, 2008. Accessed November 28, 2010
- ↑ Apprehension Test [Video]. YouTube. http://www.youtube.com/watch?v=gLBX8vUnCo0. Published June 2, 2007. Accessed November 28, 2010.
- ↑ 24.0 24.1 24.2 24.3 24.4 Handoll HHG, Al-Maiyah MA. Surgical versus non-surgical treatment for acute anterior shoulder dislocation.Cochrane Database of Systematic Review. 2004;1:1-37.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 Deyle G, Nagel K. Prolonged immobilization in abduction and neutral rotation for a first-episode anterior shoulder dislocation. Journal of orthopedic sports physical therapy. 2007; 37(4): 192-198.
- ↑ Gibson K, Growse A, Korda L, Wray E, MacDermid J. The effectiveness of rehabilitation for nonoperative management of shoulder instability: a systematic review. Journal of Hand Therapy. 2004; 17(2): 229-242
- ↑ 27.0 27.1 Robinson M, Howes J, Murdoch H, Will E. Graham C. After primary traumatic anterior shoulder dislocation in young patients. The Journal of Bone Surgery. 2006;88(11): 2326-2336.
- ↑ 28.0 28.1 Mahaffey B, Smith P. Shoulder instability in young athletes. American Family Physician. 1999;59(10): 2773-2782.