Thoracic Instability
Original Editors - Assia Dad Soumaya Ajattar Gülcan KaratasSefora Bakkiouias part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Kim Jackson, Rachael Lowe, Sefora Bakkioui, Lucinda hampton, Admin, Rani Vetsuypens, Mohit Chand, Esraa Mohamed Abdullzaher, WikiSysop and Evan Thomas
Definition/Description[edit | edit source]
Excessive motion of vertebral bodies in relation to one another is considered spinal instability (i.e. a loss of the functional integrity of a system which provides stability). Some motion is, of course, normal.
- Motion can be described as instability when the motion is significantly greater than that at adjacent levels.
- Spinal instability can be the result of an injury, degenerative process, tumor, previous surgery or congenital condition.
- Symptoms of spinal instability may include neck or back pain, nerve pain and muscle spasms[1].
- This condition often develops when a particular disc or facet joint degenerates to the point that it can no longer support the weight of the body through that segment of the spine.
- The osteoarticular ligamentous and the myofascial are two systems in the thorax that contribute stability. In the midthorax the rotational instability involves the spinal and costal components of the segment.[2] [3] [4]
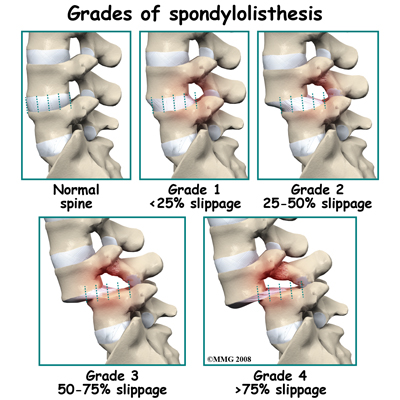
Instability in thoracic spines (if present) manifests as spondylolisthesis (forward translation of the cephalad vertebra on the caudal one).
Lateral listheses in thoracic spines are rare, possibly due to restraints provided by the rib cage and the uncovertebral joints.
The degenerative thoracic spondylolisthesis is uncommon, as the thoracic spine is inherently more stable in the anterior to posterior direction than the cervical or lumbar. This is due to the rib cage and the coronal orientation of the facet joints.
Clinically Relevant Anatomy[edit | edit source]
To understand how both mechanisms cause instability, it is important to understand the anatomy of the vertebral motion segment.
Each level of your spine functions as a three-joint complex.
- There are two facet joints in the back and a large disc that acts as a joint in front.
- This tripod creates great stability, supports the weight above each level and provides support for movement in all directions.
- As long as the disc remains healthy, it can withstand these forces for many years without any symptoms[5].
- When the posterior elements and bilateral costovertebral joints are destroyed, the thoracic spine may become unstable.
Thoracic spine additional points
- The costovertebral joints are important stabilizers of the thoracic spinal motion segments. [6] [3]
- The rib cage is fixed to the thoracic spine by the costovertebral joints.
- Thoracic vertebrae are connected to adjacent vertebrae by the bilateral costovertebral joints.
- The costovertebral joints and their surrounding ligaments, such as the costotransverse, superior costotransverse, radiatie, and intra-articular ligaments, connect nearby vertebrae and ribs. [6]
- The stabilization role of the costovertebral joints and rib cage in the thoracic spine is particularly evident in lateral bending and axial rotation.
Etiology[edit | edit source]
This instability is called spondylolisthesis which literally means the forward slippage of one lumbar vertebra in relation to the vertebra below.
Spondylolisthesis can be caused by several mechanisms. The two main causes are:
- Stress fracture in the vertebra called spondylolysis
- Acquired degenerative changes in the facet joints.[5]
Spondylolysis[edit | edit source]
A stress fracture occurs through the fragile “pars” of the vertebrae and is often broken on both sides.
- The fracture may be the result of a direct trauma, by a focused strain usually from athletic activity, or from a genetic weakness in this area of the bone.
- The pars are a thin part of the vertebrae that can break with repeated use; imagine a paperclip that has been bent over and over and finally breaks. Most commonly, a pars stress fracture occurs as an adolescent; it is estimated up to 5-7% of adolescents have a pars fracture.
- It is extremely commonly in athletes in high impact sports and those experiencing rotational forces. (Mostly seen in basketball players as the mechanism of injury involves extension with rotation at the vertebrae).
- Fortunately, these fractures often heal with a period of rest and core strengthening.
- If the bone does not heal, fibrous scar tissue may form to still provide support.
For many people this fracture does not cause problems for decades. Over time, the decreased posterior support causes more forces to be placed on the disc in front which can accelerate degenerative disc disease. When a disc narrows from degeneration, the bones above and below the disc can also move or slip on each other. The fracture gap can thus widen, causing the vertebra to shift more forward. This movement indicates segmental spinal instability.
Degenerative Changes in the Facet Joints[edit | edit source]
The other main cause of spondylolisthesis is from acquired degeneration of the facet joints. As these joints degenerate the small supporting ligaments wear out and become loose. These ligaments are essential for support. This laxity allows the facet joints to open more, or separate, with movement. The facet joints can be a source of pain and allow the disc to slip forward since the joint is separating more than it should[5].
Diagnostic Procedures[edit | edit source]
A complete history and physical exam are always the first part of a diagnostic workup for any painful condition.
- Usually, spinal x-rays will be obtained to evaluate for instability. The client will flex forward and extend backward for different x-rays to evaluate whether the bones move abnormally when you change body positions.
- Advanced imaging studies such as a CT scan or an MRI scan may also be ordered to get additional information about the amount of nerve compression that may be resulting from the instability and to see whether there are any fractures in the bony structures that might lead to the instability[1].
Medical Management[edit | edit source]
- In the setting of minimal pain without any nerve impingement, treatment of spinal instability will be aimed at conservative measures. This may involve physical therapy for core muscle strengthening, use of NSAIDs or pain medications, and probable activity modification.
- If instability creates severe pain or leads to arm or leg pain, spinal injections may also be considered to help decrease the discomfort.
- If pain is not alleviated with conservative treatment or in cases where instability results in significant compression of the spinal cord or spinal nerves, surgery is generally recommended. Although the specifics of surgery are individualized based on a given patient’s findings, generally surgical fusion is recommended.[1]
Physical Therapy Management[edit | edit source]
- The physiotherapy management of thoracic instability involves various interventions, including core muscle strengthening, manual therapy, and exercise.
- Conservative management is typically attempted as the first-line treatment, focusing on improving overall postural stability and addressing muscle imbalances.
- Manual interventions such as joint mobilization and manipulation can be used to address joint hypomobility, while exercises are aimed at improving thoracic spine mobility and stability. Additionally, the use of NSAIDs or pain medications, activity modification, and other modalities such as heat therapy, massage, and acupuncture may be considered to alleviate symptoms. It is important to individualize the treatment approach based on the specific clinical presentation and patient's needs.
- The evidence-based approach to physiotherapy management of thoracic instability is supported by research indicating the benefits of manual therapy and exercise in addressing thoracic spine pain and dysfunction. A combination of manual therapy techniques and neuromuscular control exercises has been shown to be effective in improving stability, mobility, and skill level impairments in individuals with thoracic instability. Furthermore, the use of proper technique and focus on stretching and strengthening specific muscle groups have been highlighted as important considerations in the rehabilitation process. [5]The multifidi and erector spinae muscles contribute to force closure of the midthoracic region. Therefore, it is really important that these muscles have to be addressed in the rehabilitation of the unstable thorax. The region can become dynamically stable, and the neutral zone can be controlled, through appropriate training. [2] [3]
- An exercise programs example - 10 min- warm-up exercises, 40 min-stabilization exercises, 10 min-cool-down, and stretching exercises in a group set-up. If needed a gymnastic ball or proprioceptive, balance and resistive work can be integrated into the program. The exercise velocity can be increased according to the patients work and recreation demands. The load should be applied bilaterally and then progressed to unilateral work. [7]
The program consists of:
- General exercises for the spine: The contraction of the related muscle activity according to the spine segment with the usage of Stabilizer Pressure Biofeedback unit (Chattanooga, USA). The training programs aimed at creating neutral spine and activation of deep muscles of the spine.
- Specific exercises for the thoracic spine: Postural alignment and minimal multifidus activation with scapular orientation for thoracic group. The participants were asked to maintain the positions and contractions during the exercises and throughout the day as much as possible.
- Abdominal bracing was also shown to be one of the most effective exercise techniques for muscles even compared to dynamic exercises involving trunk flexion/ extension movements. Furthermore, abdominal bracing should be included in exercise programs when the goal is to improve trunk stability. Moreover, abdominal bracing also shows an increase in stiffness of the spine, promoting stability in the vertebral segments, and is frequently recommended and/or included in rehabilitation. Further investigation focusing on its actual effects on spinal stability in rehabilitation is needed. [8] [9] . Also, along Skoch, Jesse et al. further investigation is needed to determine when and if (post operative) bracing for surgically stabilized thoracolumbar fractures is indicated. Controlled studies should include a careful analysis of pseudoarthrosis and complication rates. [10]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Beazell, J. R., Mullins, M., & Grindstaff, T. L. (2010). Lumbar instability: An evolving and challenging concept. The Journal of Manual & Manipulative Therapy, 18(1), 9-14.
- ↑ 2.0 2.1 D.G. Lee, Rotational instability of the mid-thoracic spine : assessment and management, 1996, Manual Therapy
- ↑ 3.0 3.1 3.2 O'Sullivan, Peter B. "Masterclass. Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management." Manual therapy 5.1 (2000): 2-12.
- ↑ Panjabi, Manohar M., Jeff N. Hausfeld, and Augustus A. White. "A biomechanical study of the ligamentous stability of the thoracic spine in man." Acta Orthopaedica Scandinavica 52.3 (1981): 315-326.
- ↑ 5.0 5.1 5.2 5.3 Ribaudo, A. (2013). Management of a Patient with Lumbar Segmental Instability Using a Clinical Predictor Rule. HSS Journal, 9(3), 284-288.
- ↑ 6.0 6.1 I. Oda et al, Biomechanical role of posterieur elements, costovertebral joints, and rib cage in the stability of the thoracic spine, 1996, Spine
- ↑ D.O. Kaya et al, Effects of different segmental spinal stabilization exercise protocols on postural stability in asymptomatic subjects randomized controlled trial, 2012, Journal of back and musculoskeletal rehabilitation.
- ↑ S. Maeo et al, Trunk Muscle Activities during Abdominal Bracing: Comparison among Muscles and Exercises, 2013, Journal of Sports Science and Medicine
- ↑ F.J. Vera-Garcia, J.L. Elvira, S.H. Brown and S.M. McGill, Effects of abdominal stabilization maneuvers on the control of spine motion and stability against sudden trunk perturbations, J Electromyogr Kinesiol 17(5) (2007), 556-67
- ↑ Skoch, Jesse, et al. "Bracing after surgical stabilization of thoracolumbar fractures: a systematic review of evidence, indications, and practices." World neurosurgery 93 (2016): 221-228.