Temporal Arteritis (Giant Cell Arteritis)
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kiersten Young, Savannah Lane, Lucinda hampton, Elaine Lonnemann, 127.0.0.1, WikiSysop, Kim Jackson and Sehriban Ozmen
Introduction[edit | edit source]
Temporal arteritis, also known as giant cell arteritis (GCA), is a systemic inflammatory vasculitis that affects medium-sized to large arteries.[1]
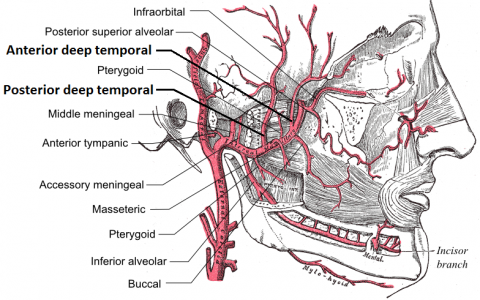
- The main arteries involved include the medium-sized muscular arteries, such as the cranial and extracranial branches of the carotid artery.
- This condition is known as a condition of the elderly and is a significant cause of secondary headache in older adults.
- GCA is closely linked to polymyalgia rheumatica (PMR), a systemic rheumatic inflammatory disorder with unknown causes[2].
- GCA and PMR usually occur together in the same patient[1].
Etiology[edit | edit source]
The exact etiology of GCA is currently unknown, various possibilities have been hypothesized
- Genetic,
- Environmental
- Autoimmune
- An association with Toll-like receptor 4 gene polymorphism as well as HLA-DR4, has been identified[3]
- It is believed that the basis for the disease involves abnormalities of the arterial elasticum, with a decreased in integrity of the inner elastic membrane of affected arteries, resulting in a giant cell reaction near this elasticum.
- Another theory is that the initial lesion is a destruction of the muscular layers of the artery’s tunica media caused by ischemia, which leads to fragmentation of the elasticum with formation of giant cells occurring secondarily[4].
Epidemiology[edit | edit source]
- GCA is the most frequent primary vasculitis, which predominantly affects Caucasian people over the age of 50[1][5].
- 95% of cases occur in patients older than 55 years[6][4].
- The incidence of GCA in 70-79 year olds is 29.6 per 100,000 individuals[7].
- Women are 2-6 times more likely to be affected than men[1][4][8].
- Giant cell arteritis occurs in at least 25% of all cases of polymyalgia rheumatica (PMR)[2].
- GCA is more frequent among people of Scandinavian and Northern European descent[1][5].
Characteristics/Clinical Presentation[edit | edit source]
The patient will usually present with complaints of a headache, painless vision loss, jaw claudication, fatigue, fever, anorexia, or temporal artery tenderness.
Patients may state that their headache has been occurring for a duration of 2 to 3 months and worsens with exposure to cold and at night when the pressure of the pillow causes pain to the artery.
- On physical exam, the temporal artery may be thickened, painful, nodular, or erythema may occur on the overlying skin.
- The temporal artery may not necessarily be the artery involved which further complicates the diagnosis.
- Many patients will present with signs or symptoms of TIA or stroke.
- The ophthalmologic exam will generally be benign, although if the circulation of the optic nerve is involved, the patient may display an afferent pupillary defect.
- Because of the inconsistencies regarding the history and physical, temporal arteritis is often a difficult disease to diagnose in the emergency setting.[3]
Associated Co-morbidities[edit | edit source]
- Polymyalgia Rheumatica (PMR)
- Visual Disturbances
- Facial pain
- Osteoporosis
- Hypokalemia
- Various infections such as oral/esophageal thrush
- Herpes Zoster[9]
Treatment[edit | edit source]
The timing of treatment is critical in these patients to prevent vision loss.
- Steroids should be started immediately upon suspicion of temporal arteritis.
- Although there is no consensus among physicians regarding the amount of steroid therapy to begin, 60 milligrams of prednisone PO or 1 mg/kg daily can be used as a general guideline. This may be required for 1 to 2 years.
- The patient should be followed by their primary care physician with frequent ESR draws.
- If acute vision loss is present, the patient may be started on 250 mg to 1000 mg of intravenous (IV) steroids for 3 days.
- Low-dose aspirin should also be started daily.
- A rheumatologist should be consulted immediately upon starting steroid treatment and before performing a biopsy.
- An ophthalmologist should also see the patient to perform a full eye exam to rule out other serious causes of vision loss[3].
Evaluation[edit | edit source]
American College of Rheumatology classification criteria for giant cell arteritis- at least three of five must be met
1. Age at onset 50 years or more
2. New-onset headache or localized headache
3. Tenderness or decreased pulsation in at least one of the temporal arteries
4. Erythrocyte sedimentation rate 50 mm/h or more
5. Abnormal artery biopsy with either mononuclear cell infiltrate or granulomatous inflammation (with giant cells)[1][5][8]
Physical Therapy Management[edit | edit source]
Physical Therapists should be aware of associated signs and symptoms and refer patients accordingly.
- Prompt initiation of treatment may prevent blindness and other ischemic related consequences.
- There are no current physical therapy treatment options for temporal arteritis and best management described in literature involves use of corticosteroids.
- The most important thing for physical therapists to be aware of are the clinical examination findings that are often associated with GCA. These include palpation of the temporal artery, auscultation of arteries including the subclavian and axillary, and bilateral blood pressure determination, looking for a predominant unilateral vascular stenosis[10]
Prognosis[edit | edit source]
GCA is a systemic disease of variable presentation and duration.
- In some patients, it has a course of a few years, while in others, the course is more chronic.
- The majority of the patients taper and discontinue the steroids after a few years of the disease, but some may require long term administration.
- These patients are at risk of side effects of glucocorticosteroids and should be closely monitored.
- GCA does not affect the overall survival rate of an individual except for those patients with aortitis and aortic dissection involvement[3]
Differential Diagnosis[edit | edit source]
- Central retinal artery occlusion
- Acute glaucoma
- Uveitic glaucoma
- Retrobulbar optic neuritis
- Orbital abscess
- Ophthalmic migraine
- Tolosa hunt syndrome
- Orbital and cavernous sinus compressive lesions
- Migraine headache
- Lyme disease
- Herpes zoster ophthalmicus
- Trigeminal neuralgia
- Diabetes
- Poorly Controlled hypertension
- Stress related disorders
- Angina pectoris [6][7]
Case Reports/ Case Studies[edit | edit source]
1. Colin G, Dupont M. Giant cell arteritis. Journal of the Belgian Society of Radiology. 2013;96(5):290.
http://br.ubiquitypress.com/articles/10.5334/jbr-btr.406/galley/403/download/
2. Lockhart M, Robbin M. Case 58: Giant Cell Arteritis1. Radiology. 2003;227(2):512-515.
http://pubs.rsna.org/doi/pdf/10.1148/radiol.2272010487
3. De Hertogh W, Vaes P, Versijpt J. Diagnostic work-up of an elderly patient with unilateral head and neck pain. A case report. Manual Therapy. 2013;18(6):598-601.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Chew S, Kerr N, Danesh-Meyer H. Giant cell arteritis. Journal of Clinical Neuroscience. 2009;16(10):1263-1268
- ↑ 2.0 2.1 Goodman C, Snyder T. Differential diagnosis for physical therapists. St. Louis, Mo.: Saunders/Elsevier; 2013.
- ↑ 3.0 3.1 3.2 3.3 Ameer MA, Peterfy RJ, Bansal P, Khazaeni B. Temporal (Giant Cell) Arteritis. StatPearls [Internet]. 2020 Jan.Available from: (last accessed 20.9.2020)https://www.ncbi.nlm.nih.gov/books/NBK459376/
- ↑ 4.0 4.1 4.2 Gurwood A, Malloy K. Giant cell arteritis. Clinical and Experimental Optometry. 2002;85(1):19-26.
- ↑ 5.0 5.1 5.2 Salvarani C, Cantini F, Hunder G. Polymyalgia rheumatica and giant-cell arteritis. The Lancet. 2008;372(9634):234-245.
- ↑ 6.0 6.1 Kawasaki A, Purvin V. Giant cell arteritis: an updated review. Acta Ophthalmologica. 2009;87(1):13-32.
- ↑ 7.0 7.1 Smith J, Swanson J. Giant Cell Arteritis. Headache: The Journal of Head and Face Pain. 2014;54(8):1273-1289.
- ↑ 8.0 8.1 Wang X, Hu Z, Lu W, Tang X, Yang H, Zeng L et al. Giant cell arteritis. Rheumatol Int. 2008;29(1):1-7.
- ↑ Petri H, Nevitt A, Sarsour K, Napalkov P, Collinson N. Incidence of Giant Cell Arteritis and Characteristics of Patients: Data-Driven Analysis of Comorbidities. Arthritis Care & Research. 2015;67(3):390-395
- ↑ Ness T, Bley TA, Schmidt WA, Lamprecht P. The diagnosis and treatment of giant cell arteritis. Dtsch Arztebl Int. 2013 May 23;110(21):376-86.