Pancreatitis
Original Editors - Amy Dean from Bellarmine University's Pathophysiology of Complex Patient Problems project. Top Contributors - Amy Dean, Admin, Lucinda hampton, George Prudden, WikiSysop, Kim Jackson, Elaine Lonnemann, Dave Pariser, Wendy Walker, Scott Buxton and 127.0.0.1
Introduction[edit | edit source]
Pancreatitis is inflammation of the pancreas, which can either be acute (sudden and severe) or chronic (ongoing). The pancreas is a gland that secretes both digestive enzymes and important hormones. Heavy alcohol consumption is one of the most common causes of chronic pancreatitis, followed by gallstones.
- Pancreatitis is one of the least common diseases of the digestive system. Treatment options include abstaining from alcohol, fasting until the inflammation subsides, medication and surgery[1].
- Pancreatitis is a potentially serious disorder characterized by inflammation of the pancreas that may cause autodigestion of the organ by its own enzymes. This disease has two manifestations: acute pancreatitis and chronic pancreatitis[2]
- Acute pancreatitis (AP) is an acute response to injury of the pancreas. Chronic pancreatitis (CP) can result in permanent damage to the structure and endocrine and exocrine functions of the pancreas.[3]
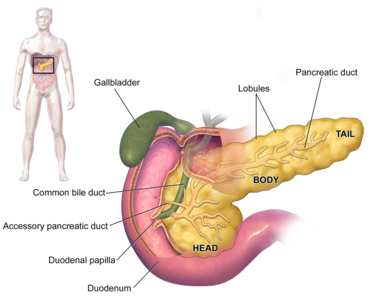
Image 1: Anatomy of the pancreas and its related organs, the gall bladder and duodenum
Acute Pancreatitis[edit | edit source]
Acute pancreatitis is the result of an inflammatory process involving the pancreas caused by the release of activated pancreatic enzymes.
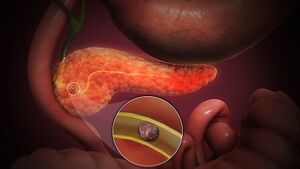
Image 2: 3D animation Acute pancreatitis
In addition to the pancreas, this disorder can also affect surrounding organs, as well as cause a systemic reaction. This form of pancreatitis is generally brief in duration, milder in symptom presentation, and reversible. However, while this form of the disease resolves both clinically and histologically, approximately 15% of patients with acute pancreatitis will develop chronic pancreatitis.[2][4] Acute pancreatitis may present as mild or severe. Milder forms of acute pancreatitis involve only the interstitium of the pancreas, which accounts for 80% of all cases, and has a temperate presentation with fewer complications. However, severe forms involve necrosis of the pancreatic tissue, which occurs in 20% of cases, and results in increased complications and mortality.[2][4]
Chronic Pancreatitis[edit | edit source]
Chronic pancreatitis develops from chronic inflammation of the pancreas that results in irreversible and progressive histologic changes. This includes fibrosis and ductal strictures, which destroy the pancreas directly, as well as decreased endocrine and exocrine functions, which can negatively affect other body systems. Unlike acute pancreatitis, this form of the disease is characterized by recurrent or persistent symptoms.[2][4]
Etiology[edit | edit source]
Around half of all people with acute pancreatitis have been heavy drinkers, which makes alcohol consumption one of the most common causes. Gallstones cause most of the remaining cases. In rare cases, pancreatitis can be caused by:
- trauma or surgery to the pancreas region
- inherited abnormalities of the pancreas
- inherited disorders of metabolism
- viruses (particularly mumps)
- medication (including some diuretics), which can also trigger inflammation[1].
Epidemiolgy[edit | edit source]
Acute pancreatitis accounts for about 275,000 hospital admissions annually.
- Eighty percent of patients admitted with pancreatitis usually have mild disease and can be discharged within a few days.
- Overall mortality of acute pancreatitis is approximately 2%.
- The relapse rate of acute pancreatitis is between 0.6% to 5.6%, and this depends on the etiology of pancreatitis. The relapse rate is highest when pancreatitis is due to alcohol use.
Chronic pancreatitis has an annual incidence rate of 5 to 12 per 100,000 people.
- The prevalence of chronic pancreatitis is 50 per 100,000 people.
- The most common age group is 30 to 40 years, and it occurs more in men than women[3].
Characteristics/Clinical Presentation[edit | edit source]
Abdominal pain is the most common presenting complaint of AP and can occur with nausea and vomiting. Chronic pancreatitis can present with or without abdominal pain, nausea or vomiting. Patients with chronic pancreatitis can present with steatorrhea and weight loss[3].
1.Common symptoms of an acute pancreatitis include: severe abdominal pain, often spreading through into the back; bloating; fever; sweating; nausea; vomiting; collapse.
2. Some people with chronic pancreatitis suffer recurrent or even constant abdominal pain, which may be severe. Other symptoms include steady weight loss, caused by the body’s inability to properly digest and absorb food. If much of the pancreas has been damaged, loss of insulin production can cause diabetes. Chronic pancreatitis can contribute to the development of pancreatic cancer.[3]
Associated Co-morbidities[edit | edit source]
Acute Pancreatitis
- Alcoholism
- 15% of patients with acute pancreatitis develop chronic pancreatitis
- 5-7% mortality rate for milder forms with inflammation confined to the pancreas
- 10-50% for severe forms with necrosis and hemorrhage of the gland and a systemic inflammatory response
- Infection of necrotic pancreatic tissue may occur after 5-7 days 100% mortality for pancreatic infection without extensive surgical debridement or drainage of the infected area
- Patients with peripancreatic inflammation or one area of fluid collection have a 10 to 15% chance of abscess formation
- Patients with two or more areas of fluid collection have a 60% incidence of abscess formation
- Diabetes mellitus (increased risk in alcoholic pancreatitis)
- Recurrent episodes (increased risk in alcoholic pancreatitis)[4][2]
Chronic Pancreatitis
- Alcoholism
- Cystic fibrosis
- Diabetes mellitus develops in 20-30% of patients within 10-15 years of onset
- Pancreatic cancer develops in 3% to 4% of patients
- Chronic disability
- 70% 10-year survival rate
- 45% 20-year survival rate
- 60% mortality rate for patients with alcohol-related chronic pancreatitis who do not cease alcohol intake[2]
Diagnosis[edit | edit source]
Pancreatitis is generally diagnosed quickly, by examination of the abdomen, and confirmed using a series of medical tests including:
- General tests – such as blood tests, physical examination and x-rays.
- Ultrasound – sound waves form a picture that detects the presence of gallstones.
- CT scan – a specialised x-ray takes three-dimensional pictures of the pancreas.
- MRI scan – this uses a strong magnetic field rather than radiation to take pictures of the abdomen. A special form of MRI called MRCP can also be used to get images of the ducts of the pancreas and help determine the cause of pancreatitis and the extent of damage[1].
Treatment[edit | edit source]
Treatment depends on the causes and severity of the condition.
Treatment for acute pancreatitis may include:
- hospital care – in all cases of acute pancreatitis
- intensive care in hospital – in cases of severe acute pancreatitis
- fasting and intravenous fluids – until the inflammation settles down
- pain relief – adequate pain relief is essential and is often given into the vein (intravenously). With appropriate pain relief, a person with pancreatitis is able to draw deep breaths, which helps to avoid lung complications such as pneumonia
- endoscopy – a thin tube is inserted through your oesophagus to allow the doctor to see your pancreas. This device is used to inject dye into the bile ducts and pancreas. Gallstones can be seen and removed directly
- surgery – if gallstones are present, removing the gallbladder will help prevent further attacks. In rare cases, surgery is needed to remove damaged or dead areas of the pancreas
- lifestyle change – not drinking alcohol.
Treatment for chronic pancreatitis may include:
- lowering fat intake
- supplementing digestion by taking pancreatic enzyme tablets with food
- cutting out alcohol
- insulin injections, if the endocrine function of the pancreas is compromised
- analgesics (pain-relieving medication)[1]
Physical Therapy Management[edit | edit source]
Acute Pancreatitis
Patients with acute pancreatitis may seek physical therapy treatment with a chief complaint of back pain.
- Back pain is common in patients with pancreatitis, as the inflammation and scarring associated with this disease can lead to decreased spinal extension, particularly in the thoracolumbar junction. This decrease in motion is difficult to treat even with patient compliance and resolution of inflammation due to the depth of the scarring. This tissue is often difficult to penetrate with mobilization techniques and, therefore, continues to decrease motion. Despite this, pain may be relieved through the use of heat to decrease muscular tension, relaxation techniques, and specific positioning techniques, including leaning forward, sitting up, or lying on the left side in the fetal position.
- It is important to note that a patient may present to physical therapy prior to a diagnosis of acute pancreatitis with back pain. While acute pancreatitis is associated with gastrointestinal symptoms, including diarrhea, pain after eating, anorexia, and unexplained weight loss, the patient may not recognize the importance or necessity of reporting what they may believe are unrelated symptoms. Therefore physical therapists must thoroughly question patients about all body systems and warning signs.
- It is also important to know that pancreatitis is frequently associated with diabetes mellitus. Over 23 million Americans are currently living with diabetes, many of which will seek physical therapy services. Because of this it is important to be aware of the signs of symptoms of pancreatitis, as patients with diabetes are at an increased risk for this condition.[5]
- Patients with acute pancreatitis my also need physical therapy services if acute respiratory distress syndrome (ARDS) develops as a complication. Assisted respiration and pulmonary care are critical interventions for these patients.
- For patients who are receiving acute care and are restricted from eating or drinking in order to let the pancreas rest, even ice chips can stimulate enzymes and increase pain. Therefore, physical therapists must be careful to follow all medical orders and not adhere to patient requests until approved by the nursing or medical staff.
- Hospitalized patients with acute pancreatitis must also be monitored for signs and symptoms of bleeding, including bruising.[2]
Chronic Pancreatitis
- Similar to acute pancreatitis, patients with chronic pancreatitis may present to physical therapy with complaints of pain in the upper thoracic spine or at the thoracolumbar junction, while those with alcohol-related chronic pancreatitis may have symptoms of peripheral neuropathy. Because patients may complain of these seemingly musculoskeletal problems, it is imperative that physical therapists receive a complete history perform a thorough examination to screen for this disease. If this visceral problem is not determined upon initial evaluation, failure to improve with therapeutic intervention necessitates referral.
- Patients with known pancreatitis or post-pancreatectomy may need physical therapy services such as monitoring vital signs and/or blood glucose levels depending on what complications exist.
- Physical therapists should also educate these patients about the effects of malabsorption and associated osteoporosis that they may experience.[2]
Differential Diagnosis[edit | edit source]
Acute Pancreatitis[edit | edit source]
Disorders presenting with symptoms similar to those of acute pancreatitis includeperforated gastric or duodenal ulcer, mesenteric infarction, medications, strangulating intestinal obstruction, dissecting aneurysm, biliary colic, appendicitis, diverticulitis, inferior wall myocardial infarction, tubo-ovarian abscess, renal failure, salivary gland disease, hematoma of the abdominal muscles or spleen, cholecystitis, vascular occlusions, pneumonia, hypertriglyceridemia, hypercalcemia, infection, post-traumatic injury, pregnancy, and diabetic ketoacidosis.[4][6][7][8]
Chronic Pancreatitis[edit | edit source]
Patients who do not present with a typical history of alcohol abuse and frequent episodes of acute pancreatitis, pancreatic malignancy must be ruled out as the cause of pain. In addition, chronic pancreatitis may initially be confused with acute pancreatitis because the symptoms are similar, gallstones, and neoplastic or inflammatory masses.[4][6]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 better health Pancreatitis Available:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pancreatitis (accessed 3.9.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. Saint Louis, MO: Saunders; 2009.
- ↑ 3.0 3.1 3.2 3.3 Mohy-ud-din N, Morrissey S. Pancreatitis.2019 Available: https://www.statpearls.com/articlelibrary/viewarticle/26577/(accessed 3.9.2021)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Beers MH, et. al. eds. The Merck Manual of Diagnosis and Therapy. 18th ed. Whitehouse Station, NJ: Merck Research Laboratories; 2006.
- ↑ American Diabetes Association. http://www.diabetes.org/ (accessed 11 April 2010).
- ↑ 6.0 6.1 Cleveland Clinic: Center for Continuing Education. Chronic Pancreatitis. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/gastroenterology/chronic-pancreatitis/ (accessed 21 March 2010).
- ↑ Carroll J, Herrick B, Gipson T. Acute Pancreatitis: Diagnosis, Prognosis, and Treatment. Am Fam Physician. 2008 Mar 1;77(5):594. http://www.aafp.org/afp/2007/0515/p1513.html (accessed 21 March 2010).
- ↑ The Department of Anaesthesia and Intensive Care. Acute Pancreatitis. http://www.aic.cuhk.edu.hk/web8/acute_pancreatitis.htm (accessed 21 March 2010).