Lumbar Compression Fracture
Top Contributors - Remko De Smedt, Ivakhnov Sergei, Andreas De Feyter, Lucinda hampton, Kim Jackson, Lien Hennebel, Lauren Lopez, 127.0.0.1, Rachael Lowe, Sam Verhelpen, WikiSysop, Aminat Abolade, Alexander Ghyssels and Joshua Samuel
Definition/Description[edit | edit source]
Fractures of lumbar vertebrae occur in the setting of either severe trauma or pathologic weakening of the bone, see image R L4 compression fracture.
- Osteoporosis is the underlying cause of many lumbar fractures, especially in postmenopausal women.
- Osteoporotic spinal fractures are unique in that they may occur without apparent trauma.
- Any injury that changes the shape of a lumbar vertebra will alter the lumbar posture, increasing or decreasing the lumbar curve.
- Most of the fractures occur at the thoracolumbar junction. [1][2]
Osteoporotic spine fractures can be graded based on vertebral height loss as:
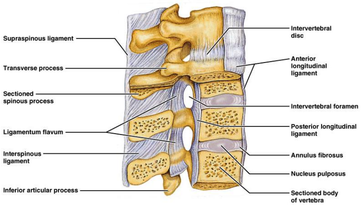
Clinically Relevant Anatomy[edit | edit source]
The figure on the right gives an illustration of the anatomy of the lumbar spine:
The lumbar vertebrae are the 5 largest and strongest of all vertebrae in the spine and the strongest stabilizing muscles of the spine attach to the lumbar vertebrae. This anatomical structure offers them the opportunity to bear the whole upper body.
The lumbar vertebrae:
- Start at the thoracolumbar junction and extend to the promontorium of the sacrum.
- Are “stacked” together and can provide a movable support structure while also protecting the spinal cord from injury.
- Have a greater mobility in flexion and extension.
- Involved in lateroflexion and rotation of the spine, but to a lesser extent.[5]
- Because of the increased mobility, the lumbar spine is more susceptible to injury. The lumbar disk works as a cushion for the mechanical loads.[6]
Epidemiology / Risk factors[edit | edit source]
Compression fractures are caused by trauma, osteoporosis, infection and neoplasm.[2][7][8]
- Most of the fractures occur at the thoracolumbar junction. This is a transition zone (T12-L2): the thoracic vertebrae are more rigid in compare to the mobile lumbar region which means that the transition zone receives the biggest load during impacts.
- > than 80 years (40% of the women at this age have received at least one compression fracture).[2][8]
- Female sex: Postmenopausal middle-aged (55-65) women go through hormonal changes which give them a higher change of developing osteoporosis.[7][9] One-fourth of the postmenopausal women will be affected with vertebral compression fractures.[10][11] The difference in incidence according to sex is nearly double for women, particularly as they age. In general, 10.7 per 1000 women have a vertebral compression fracture annually in the United States, compared with 5.7 fractures per 1000 men.[1]Bone loss is more common in women, especially post-menopausal women. This is due to the steep drop in estrogen, which goes on to makes bones lose density and become prone to fractures.
- Certain medications: eg oral steroids, anti-depressants, diabetes drugs.
- A pre-existing spinal fracture: Having one spinal fracture greatly increases your chances of having another.
- Unhealthy lifestyle habits: Smoking, excessive alcohol consumption, and/or living a sedentary lifestyle affects bone density. Smoking and heavy alcohol consumption affects your body’s ability to absorb calcium.
- Decreased pulmonary function
- Decreased mobility and balance impairment
- Multiple compression fractures. An existing compression fracture increases the risk to five-times to obtain an other compression fracture in the future. Having 2 or more compression fractures increases the risk by 12 times to get another fracture. [7]There are several patient population studies who suggests an increased mortality rate in patients with osteoporosis vertebral compression fractures that correlates with the number of involved vertebrae.[10][11]
- loss of height
- Tumour cells in the vertebra in 80% of the situations are invaded by tumor cells from the breast or prostate cancer.[2] This cancer metastasis on the vertebrae, is the most common skeletal complication in vertebral compression fractures.[10]
Characteristics/Clinical Presentation[edit | edit source]
Vertebral compression fractures (VCF)
- Most common with osteoporosis
- Possibly they are caused by high load impact trauma with a flexion compression mechanism.[12][2]
A lumbar compression fracture is a serious injury, both when caused by osteoporosis or by trauma. There is a risk of neurological damage, when this is the case, surgery is recommended,[10] Neurologic deficits are quite uncommon. [2]
- Midline back pain is the hallmark symptom of lumbar compression fractures.
- The pain is axial, non-radiating, aching, or stabbing in quality and may be severe and disabling.
- The location of the pain corresponds to the fracture site, as seen on radiographs.
- In elderly patients with severe osteoporosis, however, there may be no pain at all as the fracture occurs spontaneously.[13]
- A fracture has an influence on the quality of life and the disability can last at least 5 years and the pain for 2-4 years.
- VCFs can lead to chronic pain, disfigurement, height loss, impaired activities of daily living, increased risk of pressure sores and psychological distress.
- Patients with an acute VCF may report an abrupt onset of back pain with position changes, coughing, sneezing, or lifting.[14]
Classification of Fractures[edit | edit source]
There are several classification systems for VCF
- Wedge fracture [1][5] Burst/crush fracture [1][5] Biconcave fracture (meaning the walls of the vertebrae stays intact but the center portion is compressed).[6]
- Applied Forces of impact: [7]
- Flexion compression with damage in posterior ligamentous structures.
- Lateral compressions that can be the cause of scoliotic deformation.
- Axial compression causing burst fractures.
- Damage in the included endplate. There are four subtypes for compression fractures. [8]
| Type A: Both endplates are involved. | = Axial load | → 16% |
| Type B: The superior endplate is damaged. | = Axial load + flexion | → 62% |
| Type C: Inferior endplate is damaged | = Axial load + flexion | → 6% |
| Type D: Both endplates are intact. | = Axial load + rotation | → 15% |
Differential Diagnosis[edit | edit source]
- Coccyx pain: Coccygodynia (Coccydynia, Coccalgia, Tailbone Pain)
- Lumbar facet arthropathy: Lumbar Facet Syndrome
- Mechanical low back pain (Clinical pain presentations)
- Lumbar degenerative disc disease
- Lumbar Spondylolysis and Spondylolisthesis
- Primary OsteoporosisSecondary osteoporosis
Diagnostic Procedures[edit | edit source]
Compression fractures are typically diagnosed by lateral radiography of the vertebral column, with or without anteroposterior views. Radiographic criteria for VCFs include a decrease in vertebral body height of at least 20% or a 4-mm reduction from baseline height. The classic radiographic finding is an anterior wedge fracture.[14]
- Comparisons to pre-existing spine X-rays allows the clinician to diagnose and judge the age of the vertebral fracture.
- A plain radiograph may be all that is necessary for a majority of compression fractures, especially if one proceeds with conservative, medical management[1].
- CT scans allows for the best imaging of bony anatomy and improved assessment of loss of height, fragment retropulsion, and canal compromise. [1]
- Magnetic resonance imaging (MRI) - best study for judging fracture age. [1]
- DEXA scan: Roughly half of patients with vertebral fractures have osteoporosis (T score , −2.5) and another 40% have osteopenia (T score −1 to −2.5).
Outcome Measures[edit | edit source]
- Visual analogue scale for overall pain (VAS).
- Quality of Life Questionnaire of the European Foundation for osteoporosis (QUALEFFO).
- EQ–5D
- Roland–Morris Disability Questionnaire.
- The Patient-Specific Functional Scale (PSFS)
- Quebec Back Pain Disability Questionnaire
Medical Management[edit | edit source]
There are several medical management methods to treat a lumbar compression fracture.
Before anything else you need to control the pain:
Acute pain control may include: [1]
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Muscle relaxants
- Narcotic pain medication
- Neuropathic pain agents (ie, tricyclic antidepressants)
- Local analgesic patch
- Intercostal nerve blocks, and transcutaneous nerve stimulation units.
NSAIDs are often first-line drugs for back pain as they do not have sedating effects. However, they do have gastric toxicity and an increased risk of cardiac events for patients with hypertension and coronary artery disease [12]
Opioids and muscle relaxants may provide strong relief when NSAIDs are inadequate but have significant sedative effects as well as the risk of dependency. As such their use needs to be carefully balanced in the geriatric patient. ' [5]
Preventative Medicine[edit | edit source]
Other than acute pain control, medical therapy should be aimed at improving bone quality and thus reducing the risk of future fracture. Agents for treating osteoporosis include:
- Bisphosphonates
- Selective estrogen receptor modulators
- Recombinant parathyroid hormone
- Calcitonin
- Vitamin D
These agents act through either antiresorptive or osteogenic mechanisms.[1]
Surgical Management[edit | edit source]
Percutaneous vertebral augmentation, including vertebroplasty or kyphoplasty, can be considered in patients with inadequate pain relief from nonsurgical care, or when persistent pain substantially affects quality of life.
Recent studies have questioned their effectiveness.
- Vertebroplasty entails injecting liquid cement into a collapsed vertebral body through a needle inserted transpedicularly.
- Kyphoplasty involves percutaneously injecting a balloon into the vertebral body, inflating it to restore vertebral height, and injecting cement to reduce pain.
Complications include extravasation of cement (more common with vertebroplasty), embolism, neurologic injury, bleeding, hematoma, infection, and an increased risk of VCFs at other levels[14].
Non Medical Management[edit | edit source]
Non-operative treatment consists of[7]
- Pain relief (NSAIDs,muscle relaxants,narcotic pain medication →see medical management)
- Orthosis
- Rehabilitation program
Non-operative treatment goals[8]
- Pain control
- Early mobilisation
- Prevention of deformity
- Functional Restoration
Physical Therapy Management[edit | edit source]
Subjective Examination[edit | edit source]
Any notable event the patient experienced in the history, causing the symptoms and complaints.
High-Risk Mechanism of injury [2]
- Accident with a vehicle with a higher speed than 70 kph
- Fall from 3m or higher
- Ejection from a vehicle seat
- Check for Red Flags in Spinal Conditions
Objective Examination[edit | edit source]
It is important to know that there are no fully validated screenings for diagnosing lumbar compression fractures. Therefore radiologists have an important role in diagnosing spinal fractures.
Input from radiologists is needed because there is a lack in knowledge for diagnosing those fractures without images and the symptoms might be absent or it is difficult to determine the cause of the complaints.[2]
Inspection - Look at: [edit | edit source]
- Sagittal convexity [11] -Thoracic kyphosis, Lumbar Lordosis, Dowager’s hump (indication for osteoporosis)
- Swelling or hypertonic muscles
- Posture
- Antalgic stand
Acute phase: Localised tenderness over the involved level is a known characteristic for acute fracture. However, this does not distinguish whether the anterior or posterior column is involved. [11]
Changes in the size of the thoracic kyphosis/lumbar lordosis: [11][10]
- Can lead to a reduction of the abdominal space and/or a decreased ventilator capacity.[10]
- Can lead to multiple anterior wedge fractures: increased thoracic convexity[11]
- Can lead to an increased thoracic kyphosis with missing prevalent fracture of the vertebrae in older adults.[11]
Testing [edit | edit source]
- Active ROM- will be restricted with most acute fractures (flexion/extension/retroflexion/rotation)[10]
- Gait
- Provoking movements - flexion, extension, rotation, sneezing/coughing [11]
Specific clinical signs in physical examination:
- Patient is standing in the front of a mirror with the examiner behind him. That way the therapist can gauge their reaction. Using firm, closed-fist percussion the spine will be examined over the entire length. [11] Positive test: Patient is complaining about sharp, sudden, fracture pain.[11]Sensitivity: 87,5, Specificity: 90 %
- Patient is gently asked to take place on the examination couch and lie supine, using only one pillow.[11] Positive test: Patient is unable to lie supine, because the severe pain is the limitation factor. [11] Sensitivity: 81,25 Specificity: 93,33 %
- Physical examination reveals- tenderness when palpating or directly percussion over the area of the fracture, spasm in paraspinal muscles.[1]mostly in acute phase [11]
- Osteoporotic patients might have a loss of height. We look at the fingertips;Positive test: When the patient’s fingertips hit the knee or lower thigh during standing [11]
Note: Signs 1 and 2 are useful adjuncts in evaluation symptomatic osteoporotic vertebral compression fractures and are reliable indicators of the presence of a fracture. When the test is positive there is reason to rationalise and refer the patient for a MR scan. [11]
Treatment[edit | edit source]
Education in activities of daily living and mobility in ways to avoid pain is essential for this impaired patient population that is often elderly. [8] It is important that the patient overcomes his fear of movement (kinesiophobia) and continues with his/her activities. Rest is not recommended, it’s important that the patient remains active.[9]
Supervised Physical Therapy:[edit | edit source]
- Postural taping: from anterior aspect of each shoulder, posteriorly and obliquely down to opposite rib cag[11]
- Soft tissue massage: performed in prone to erector spinae, rhomboids, upper trapezius -stroking, circular frictions and petrissage [11]
- Strengthening-exercises: It is important to improve the lumbar stabilization by strengthening the muscles of the lower back, strengthening the patient’s supportive axial musculature (in particular the spinal extensors) but also the muscles of the trunk. Exercises should focus on strengthening back extension and may include weighted or unweighted prone position extension exercises, isometric contraction of the paraspinal muscles, and careful loading of the upper extremities. [1],[1]
- Physiotherapy program with manual techniques, clinician-led exercises, and home exercises designed to reduce pain, increase back extensor and lower limb muscle strength, and improve posture, trunk stability and trunk mobility. [11]
- The Spinal Proprioception Extension Exercise Dynamic (SPEED) program designed by Sinaki9 is an example of a regimen that focuses on strengthening the spinal extensors using a weighted kypho-orthosis and postural and proprioceptive training, through twice-daily, 20-minute exercise sessions. [2]
- Strengthening of abdominal, gluteal and hip muscles is important to support spinal structures with noncompressive forces and can be done for integrating the exercises into a more functional rehabilitation programme. Functional exercises that use all planes of motion and stimulate activities of daily living may be more beneficial for the patiënt. [8]
Example of Exercise Program: [11][edit | edit source]
| Exercise | Dosage | Weeks |
| Elbows back in sitting Hands behind head with elbows pointing out to side. Pressing elbows back by performing scapular retraction |
5 sec hold × 5 reps | 1-10 daily |
| Trunk mobility in sitting Hands on shoulders, gentle rotation in both directions and lateral flexion to each side |
5 reps in each direction | 1-10 daily |
| Four point kneeling with transversus abdominus Push into floor with hands, knees and feet then draw navel up and in. Hold 5sec |
8-10 reps × 2 |
3×/week |
| Four point kneeling with one arm and leg lift As above, then lift one arm off ground. Progress to also lifting extended leg off ground at same time |
8-10 reps × 2 | 3-10 3×/week |
| Bridging in supine Knee bent and feet flat on ground. Pushing through feet to lift back and pelvis off ground |
5-10 sec hold × 5 | 1-2 3×/week |
| Hip extension in prone 8-10 reps × 2 3-10 Raising one leg off the ground and then the other |
8-10 reps × 2 | 3-10 3×/week |
| Seated row with dumbbells Upright sitting and pull hands up towards chest by bending elbows and then lowering |
8-10 reps × 2 | 1-10 3×/week |
Patients who followed a back extensor-strengthening program have a smaller chance to relapse into a new lumbar fracture in the future.[1]
Note- if the patient continues to have a lot of pain, or there is no progression at all, it is advised to send the patient to a doctor or preferably an orthopedic surgeon for a review and possible surgery. [10]
Orthotics[edit | edit source]
The rehabilitation starts with a thoracic-lumbar-sacral orthosis. The physiotherapist learns the patient how to use that orthosis. It is recommended to wear the brace/orthosis for 6 to 12 weeks, followed by supervised physical therapy.[5]
It is important to highlight that there isn’t really any true evidence on the effectiveness of a brace in the healing of the vertebrae itself, but we can be sure a brace improves the body posture. It increases the trunk muscle strength in patients with osteoporotic fractures in the vertebrae. [2] The use of a spinal orthosis maintains neutral spinal alignment and limits flexion, thus reducing axial loading on the fractured vertebra. In addition, the brace allows for less fatigue of the paraspinal musculature and muscle spasm relief. [1]
Fractures in the thoracic spine may be treated with thoracolumbar orthesis. Examples include the Jewitt, cruciform anterior spinal hyperextension, and Taylor brace. Braces which extend to the sacrum are termed thoracolumbar sacral orthoses. Finally, lumbosacral orthoses are also available for lumbar fractures but are only effective in restricting sagittal plane motion in the upper lumbar spine (L1–3). [1] Intervertebral motion has been shown to actually increase from L4–S1 with a lumbosacral orthoses brace. [5]
Summary[edit | edit source]
- Vertebral compression fractures (VCFs) are the most common complication of osteoporosis, affecting more than 700,000 Americans annually (typical candidate R)
- Fracture risk increases with age, with four in 10 white women older than 50 years experiencing a hip, spine, or vertebral fracture in their lifetime.
- VCFs can lead to chronic pain, disfigurement, height loss, impaired activities of daily living, increased risk of pressure sores and psychological distress.
- Physical examination findings are often normal, but can demonstrate kyphosis and midline spine tenderness.
- More than two-thirds of patients are asymptomatic and diagnosed incidentally on plain radiography.
- Acute VCFs may be treated with analgesics such as acetaminophen, nonsteroidal anti-inflammatory drugs, narcotics, and calcitonin (be mindful of medication adverse effects in older patients).
- Other conservative therapeutic options include limited bed rest, bracing, physical therapy, nerve root blocks, and epidural injections.
- Percutaneous vertebral augmentation, including vertebroplasty and kyphoplasty, is controversial, but can be considered in patients with inadequate pain relief with nonsurgical care or when persistent pain substantially affects quality of life.
- Family physicians can help prevent vertebral fractures through management of risk factors and the treatment of osteoporosis.[14]
Presentations[edit | edit source]
 |
Management of Lumbar Fractures
This presentation, created by Mel Kaplan, Jacob Landersm Kari Mann, and Kelsie Martin; Texas State DPT Class. |
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 Zdeblick TA. Compression and wedge fractures: treatment and recovery. Spine Univers 2009
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Alexandru, Daniela, and William So. "Evaluation and management of vertebral compression fractures." Permanente Journal 16.4 (2012). (Level of evidence: 2A)
- ↑ Radiopedia. Osteoporotic spinal compression fracture Available from: https://radiopaedia.org/articles/osteoporotic-spinal-compression-fracture (last accessed 17.5.2019)
- ↑ Spinelive Spinal compression fractures. Available from: https://www.youtube.com/watch?v=LILgFAEMAbg (last accessed 17.5.2019)
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Kinematics of the Spine. In White AA, Panjabi MM, eds: Clinical Biomechanics of the Spine, 1990
- ↑ 6.0 6.1 Bogduk N. Clinical anatomy of the lumbar spine and sacrum. Elsevier, 2005
- ↑ 7.0 7.1 7.2 7.3 7.4 Gertzbein SD, Khoury D, Bullington A, St John TA, Larson AI. Thoracic and lumbar fractures associated with skiing and snowboarding injuries according to the AO comprehensive classi cation. Am J Sports Med 2012 Aug;40(8):1750-4. DOI: http://dx.doi. org/10.1177/0363546512449814 (Level of evidence: 2A)
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Goldstein, Christina L., et al. "Management of the elderly with vertebral compression fractures." Neurosurgery 77 (2015): S33-S45. (Level of evidence: 2A)
- ↑ 9.0 9.1 Meunier PJ. Osteoporosis: diagnosis and management. Martin Dunitz, 1998
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 Sujoy M, Yu-Po, L. Current concepts in the management of vertebral compression fractures. Oper Tech Orthop 2011; 21:251-260 (Level of Evidence 2A)
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 11.13 11.14 11.15 11.16 11.17 11.18 Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. The spine Journal 2006; 6:479-487 (Level of Evidence 1A)
- ↑ 12.0 12.1 Chieh-Tasai W, et al. Classification of symptomatic osteoporotic compression fractures of the thoracic and lumbar spine. Journal of Clinical Neuroscience 2006; 12: 31-38 (Level of Evidence 1B)
- ↑ Medscape. Lumbar compression fracture clinical presentation. Available from: https://emedicine.medscape.com/article/309615-clinical (last accessed 18.5.2019)
- ↑ 14.0 14.1 14.2 14.3 McCARTHY JA, Davis A. Diagnosis and management of vertebral compression fractures. American family physician. 2016 Jul 1;94(1):44-50. Available from:https://www.aafp.org/afp/2016/0701/p44.html (last accessed 7.6.2020)