American Spinal Injury Association (ASIA) Impairment Scale
Original Editor - Naomi O'Reilly.
Top Contributors - Naomi O'Reilly, Arnold Fredrick D'Souza, Stacy Schiurring, Kim Jackson, Jess Bell, Admin, Abbey Wright, Tarina van der Stockt, Rucha Gadgil and Olajumoke Ogunleye
Disclaimer: digital rectal examination involving deep anal pressure and voluntary anal contraction is discussed on this page. This is an invasive and advanced assessment technique and should only be performed after demonstrating competency after in-person mentorship.
Introduction[edit | edit source]
A traumatic spinal cord injury (SCI) is a life-changing event which can affect patients both physically and emotionally. The global incidence of traumatic spinal injury is approximately 10.5 cases per 100,000 persons. According to a 2022 systematic review and meta-analysis, the incidence of traumatic spinal injuries occurs in greater numbers in low- and middle-income countries (13.69 per 100,000 persons) compared to countries with high income (8.72 per 100,000 persons).[1]
For a review of spinal cord injury, please read this article.
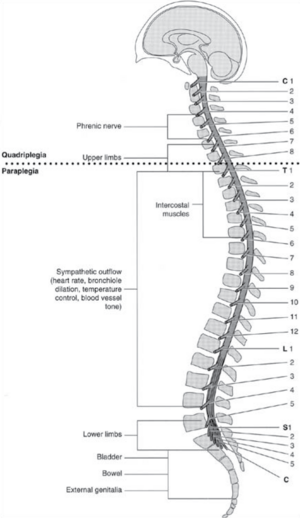
Spinal cord injury can severely impair or cease the conduction of sensory and motor signals, as well as functions of the autonomic nervous system. A systematic examination of dermatomes and myotomes allows clinicians to determine the affected segments of the spinal cord.
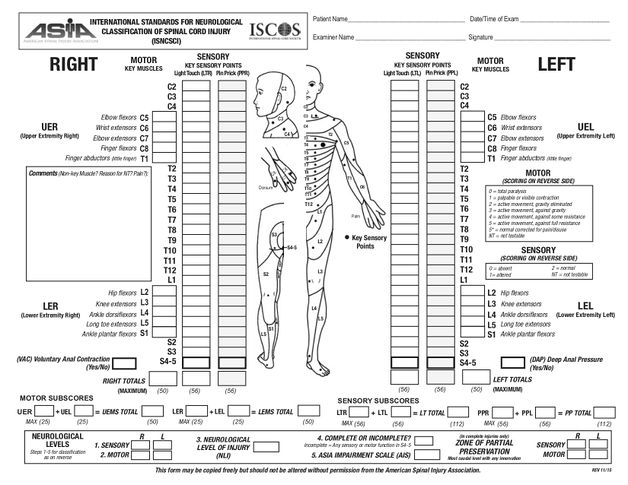
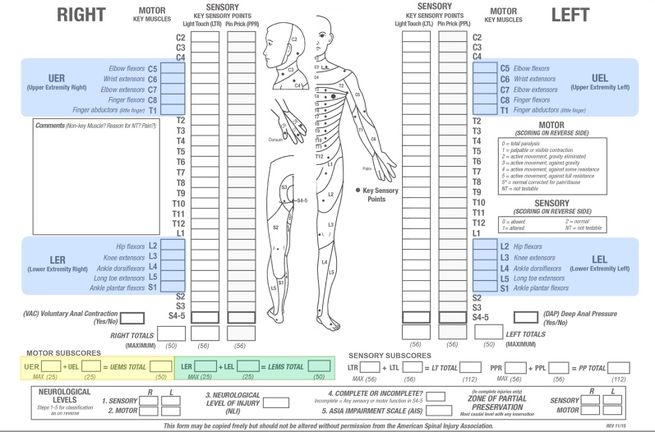
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), commonly referred to as the ASIA Exam, was developed by the American Spinal Injury Association (ASIA).[2]
The ASIA exam is a standardised physical examination consisting of a;
- myotomal-based motor examination;
- dermatomal-based sensory examination, and
- an anorectal examination.
Upon completion of these three components, an injury grade and level are assigned. This designation can then be used for rehabilitation prognosis, to guide treatment interventions, and aid in multidisciplinary communication.
The aim of the ASIA scale is to provide;
- standardised and detailed documentation of the SCI neurological level of injury;
- guidance for radiographic assessment and treatment, and
- to determine if the SCI is complete or incomplete.[3]
It should be noted that patients with an acute SCI present with spinal shock, which is "an acute state of diminished spinal function characterised by loss of all sensorimotor functions caudal to the site of injury." Spinal shock is a transient condition. Therefore, the initial neurological examination can be misleading. Continual and ongoing assessment over the days following the initial injury is vital to determine the true extent of a patient's SCI.[4]
Sensory Examination[edit | edit source]
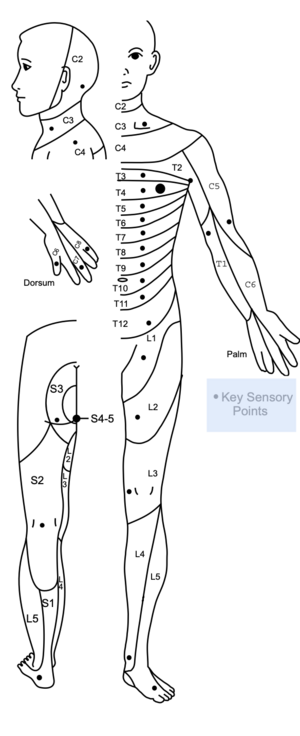
Key sensory points are readily located in relation to bony anatomical landmarks in the dermatomes C2 - S5. They are tested bilaterally using light touch (LT) and pin-prick (PP) [sharp/dull discrimination]. Equipment common in clinical settings is used, such as a cotton tip applicator for light touch and either a neuro-tip or safety pin for pin-prick. Light touch and pin prick sensation at each of the key points are compared to sensation on the patient’s cheek, which provides a normal frame of reference.[3]
Three-Point Scale for Sensory Scoring[edit | edit source]
A three-point scale is used for sensory scoring:
| 0 | = | Absent |
| 1 | = | Altered - Impaired or Partial Appreciation, including Hyperesthesia |
| 2 | = | Normal or Intact - Similar as on the cheek |
| NT | = | Not Testable |
Not testable is recorded when a key sensory point is not able to be assessed for any reason, such as a cast, burn, or amputation. When this occurs, the sensory scores for that side of the body and the total sensory score cannot be determined. The neurological level should still be determined as accurately as possible, but the sensory score and impairment grade (discussed below) should be retested and determined at a later date.
Sensory Examination Performance Tips[edit | edit source]
- Light touch sensation is tested using a wisp of cotton, which is stroked once across an area that does not exceed 1cm of skin. The patient keeps their eyes closed or has their vision blocked during testing.
- Pin-prick sensation (sharp/dull discrimination) is performed with a disposable safety pin. The pointed end is used to test for sharp discrimination and the rounded end of the pin for dull.
- When testing for pin-prick appreciation, the examiner must determine if the patient can correctly and reliably discriminate between sharp and dull sensation at each key sensory point. If in doubt, 8 out of 10 correct answers are suggested as a standard for accuracy; as this reduces the probability of correct guessing to less than 5%.
- A score of 0 is recorded if there is an inability to distinguish between dull and sharp sensation or when the patient is unable to feel when being touched by the pin.
- A score of 1 is recorded when sharp/dull sensation is impaired.
International Standards for Neurological Classification of Spinal Cord Injury Key Sensory Testing Points[edit | edit source]
Please see the additional resources section at the end of this article for video examples of dermatome testing of all key sensory points.
| Level | Description of Key Points for Sensory Testing |
|---|---|
| C2 | 1 cm lateral to occipital protuberance |
| C3 | Supraclavicular fossa at midclavicular line |
| C4 | Over acromioclavicular joint |
| C5 | Lateral side antecubital fossa just proximal to elbow crease |
| C6 | Dorsal surface of proximal phalanx of the thumb |
| C7 | Dorsal surface of proximal phalanx of the middle finger |
| C8 | Dorsal surface of proximal phalanx of the little finger |
| T1 | Medial side of antecubital fossa, just proximal to medical epicondyle of humerus |
| T2 | Apex of axilla |
| T3 | Midclavicular line and 3rd intercostal space |
| T4 | Midclavicular line and 4th intercostal space at nipple line |
| T5 | Midclavicular line and 5th intercostal space midway between T4 and T6 |
| T6 | Midclavicular line and 6th intercostal space at the level of xiphisternum |
| T7 | Midclavicular line and 7th intercostal space midway between T6 and T8 - quarter distance between the level of the xiphisternum and umbilicus |
| T8 | Midclavicular line and 8th intercostal space midway between T6 and T10 - half distance between the level of the xiphisternum and umbilicus |
| T9 | Midclavicular line and 9th intercostal space midway between T8 and T10 - three-quarters distance between the level of the xiphisternum and umbilicus |
| T10 | Midclavicular line and 10th intercostal space at the level of the umbilicus |
| T11 | Midclavicular line and 11th intercostal space midway between T10 and T12 - midway between the level of the umbilicus and inguinal ligament |
| T12 | Midclavicular line over midpoint of the inguinal ligament |
| L1 | Midway between sensory point at T12 and L1 |
| L2 | Anterior-medial thigh at the midpoint drawn connecting the midpoint of the inguinal ligament and medial femoral condyle |
| L3 | Medial femoral condyle above the knee |
| L4 | Medial malleolus |
| L5 | Dorsal foot at the 3rd metatarsal phalangeal joint |
| S1 | Lateral aspect of the calcaneus |
| S2 | Midpoint of the popliteal fossa |
| S3 | Over ischial tuberosity or infragluteal fold |
| S4 - 5 | Perianal area < 1cm lateral to mucocutaneous junction |
Information in the above table is adapted from the 2011 version of International Standards for Neurological Classification of Spinal Cord Injury.[3]
Deep Anal Pressure[edit | edit source]
The examiner’s gloved and lubricated index finger applies a gentle pressure to the internal anorectal wall, which is innervated by the somatosensory components of the pudendal nerve S4/5. Perceived pressure is graded as absent or present. Any reproducible pressure sensation felt in the anal area during this part of the examination signifies that the patient has a sensory incomplete lesion. Evaluation of deep anal pressure may not be required in individuals who have light touch or pin-prick sensation at S4-5, as they will already be designated as having a sensory incomplete injury.[3]
Special Topic: Digital Rectal Exam (DRE) in the Research
There is growing evidence that the use of the DRE in the assessment of traumatic spinal cord injury lacks validity and reliability. A 2022 systematic review by Docimo et al.[5] found that the sensitivity ranged from 0-50% for DRE in detecting both SCI and urethral injuries in adult trauma populations. This review found that the use of DRE in trauma patients has limited or no validity and reliability in assessing for spinal cord and urethral injuries, and ultimately did not influence the management of these injuries.[5]
Another study by Beeton et al.[6] found that DRE had poor sensitivity and specificity for SCI and did not recommend it as a screening tool with this patient population.
As of now, the 2019 version of the ASIA exam continues to utilise the DRE as part of SCI assessment and classification.
Sensory Level[edit | edit source]
A patient's sensory level is defined as the most caudal, intact dermatome for both light touch and pin-prick sensation. The sensory level is determined by performing an examination of the key sensory points within each of the 28 dermatomes on each side of the body, as discussed above. The sensory level is the intact dermatome level located immediately above the first dermatome level with impaired or absent light touch or pin-prick sensation. It should be determined for each side of the body as the right and left sides may differ.
Up to four sensory levels may be generated for each dermatome:
- Right pin-prick
- Right light touch
- Left pin-prick
- Left light touch
The overall single sensory level is the most rostral intact sensory point.[3]
Sensory Score[edit | edit source]
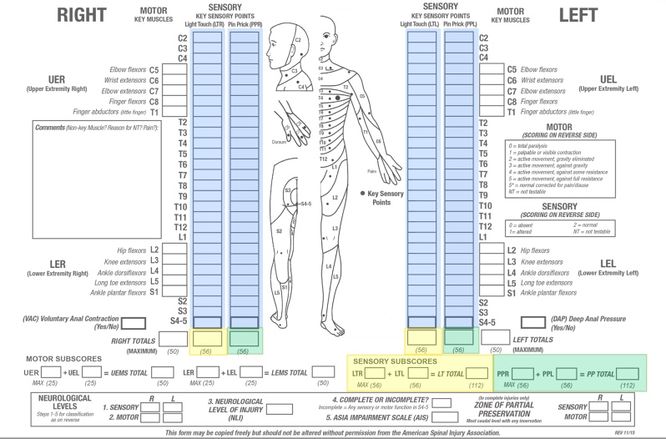
Sensory scores of each dermatome for light touch (yellow on the image above) and pin-prick (green on the image above) can be summed across dermatomes and sides of body, right and left, to generate two summary sensory scores.
- Normal sensation for each modality is assigned a score of 2. A score of 2 for each of the 28 key sensory points for light touch on each side of the body would result in a maximum score of 56 for light touch. A score of 2 for each of the 28 key sensory points for pin-prick on each side of the body would result in a maximum score of 56 for pin-prick. The total maximum sensory score is 112.
- The sensory score provides a means of numerically documenting changes in sensory function, but cannot be calculated if any required key sensory point is recorded as "not testable."[3]
Motor Examination[edit | edit source]
The motor examination involves the grading of five specific muscle groups in the upper extremities and five specific muscle groups in the lower extremities. The muscles evaluated represent the major cervical and lumbar myotomes.
Key motor testing of the 10-paired myotomes are tested bilaterally. Improper positioning and stabilisation can lead to substitution by other muscles, and will not accurately reflect the muscle function being graded.[3]
- The patient should be tested in supine, except for the rectal examination, which can be performed side-lying.
- Each key muscle function should be examined in a cephalo-caudal sequence.
- When testing, stabilise both above and below the joint to prevent muscle substitution.
- Move the joints through their full range of movement prior to completing manual muscle testing (MMT) to rule out any pain, spasticity, or contracture which might impact the scores.
Special Topic: Spinal Precautions
- Spinal precautions should be implemented in all patients who have sustained an acute traumatic injury until a spinal fracture is ruled out. Precautions include limiting flexion, extension, rotation, and twisting of the spine to avoid exacerbating an injury to the spinal cord.[7]
- The use of cervical collars for suspected cervical-level spinal fractures is a standard emergency protocol. Research shows that the use of cervical collars can elevate intracranial pressure or cerebrospinal fluid pressure, lead to skin breakdown, and increase the risk of aspiration in elderly persons. It is important to rule out cervical-level spinal injuries as soon as possible to allow for safe removal of the cervical collar.[8]
- For any patient with a suspected acute traumatic injury below the T8 skeletal level, their hip should not be allowed to actively or passively flex beyond 90° due to the increased kyphotic stress placed on the lumbar spine. Instead, a unilateral, isometric examination should be completed to ensure the contralateral hip remains extended to stabilise the pelvis.[3]
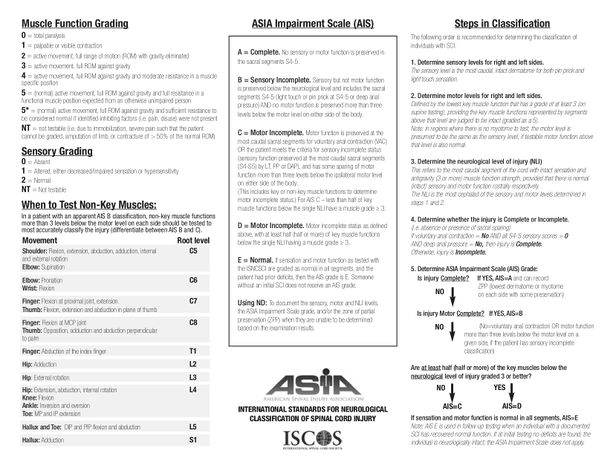
Six-Point Scale Motor Scoring[edit | edit source]
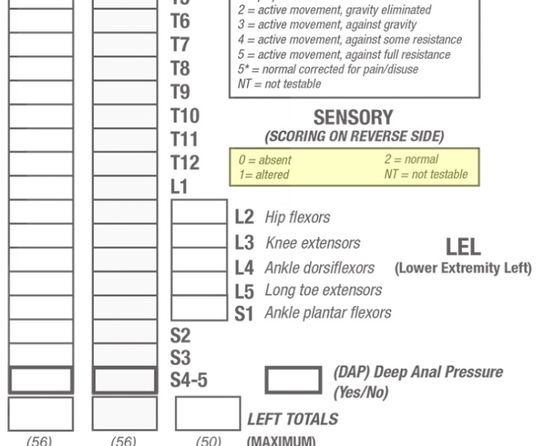
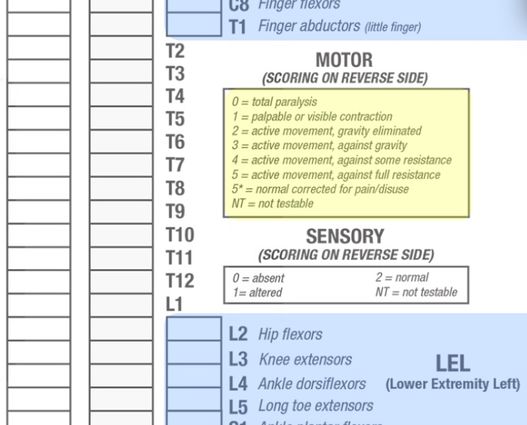
A six-point scale is used for motor scoring:
| 0 | = | Total paralysis |
| 1 | = | Palpable or visible contraction |
| 2 | = | Active movement, full range of motion with gravity eliminated |
| 3 | = | Active movement, full range of motion against gravity |
| 4 | = | Active movement, full range of movement against gravity and moderate resistance in a muscle specific position |
| 5 | = | Normal active movement, full range of motion against gravity and full resistance in a muscle specific position expected from an unimpaired person |
| 5* | = | Normal active movement, full range of motion against gravity and sufficient resistance to be considered normal if identified inhibiting factors i.e., pain, disuse were not present |
| NT | = | Not testable i.e., due to immobilisation, severe pain such that the patient cannot be graded, amputation of limb, or contracture of >50% of the range of motion |
International Standards for Neurological Classification of Spinal Cord Injury Key Motor Testing[edit | edit source]
Please see the additional resources section at the end of this article for video examples of motor testing of all 10 myotomes.
| Level | Key Muscle Function & Muscles | Description of Muscle Function Testing Position for Grade 4 or 5 |
|---|---|---|
| C5 | Elbow Flexion
|
Elbow flexed at 90 degrees, forearm supinated |
| C6 | Wrist Extension
|
Full wrist extension |
| C7 | Elbow Extension
|
Shoulder neutral rotation, adducted at 90 degrees of flexion with elbow at 45 degrees of flexion |
| C8 | Flexion of Middle Finger
|
Fully flexed distal phalanx with proximal finger joint stabilised in extension |
| T1 | Abduction of Little Finger
|
Full abduction of fingers |
| L2 | Hip Flexion
|
Hip flexed at 90 degrees |
| L3 | Knee Extension
|
Knee flexed at 15 degrees |
| L4 | Ankle Dorsiflexion
|
Full dorsiflexion |
| L5 | Long Toe Extensors
|
Full extension 1st toe |
| S1 | Ankle Plantarflexion
|
Hip neutral with full knee extension and full ankle plantarflexion |
Information in the above table is adapted from Burns et al.[3]
Voluntary Anal Contraction[edit | edit source]
The external anal sphincter is innervated by the somatic motor components of the Pudendal Nerve (S2-4). The examiner introduces a gloved and lubricated finger into the external anal sphincter and instructs the patient to “squeeze as if to hold back a bowel movement". A contraction is graded as Absent (0) or Present (1).
- A voluntary anal contraction during this part of the examination signifies that the patient has a motor incomplete injury.
- Examiners should be careful to distinguish between voluntary anal contraction from reflex anal contraction, which tends to be produced only with the Valsalva Maneuver.[3]
Motor Level[edit | edit source]
The motor level is defined by the lowest key muscle function that has a grade of at least 3 (on supine testing), provided the key muscle functions represented by segments above that level are judged to be intact (graded as a 5). As described above, the motor level is determined by examining the key muscle function within each of the ten myotomes on each side of the body. In regions where there are no clinically testable myotomes (i.e., C1 to C4, T2 to L1, and S2 to S5), the motor level is presumed to be the same as the sensory level, if testable motor function above that level is also normal.[3]
Motor Score[edit | edit source]
Motor scores for each myotome can be summed across myotomes and sides of body, right and left, to generate a single motor score for each of the upper limbs and lower limbs.
- Normal strength is assigned a grade of 5 for each muscle function. A score of 5 for each of the five key muscle functions of the upper extremity would result in a maximum score of 25 for each extremity, totalling 50 for the upper limbs. A score of 5 for each of the five key muscle functions of the lower extremity would result in a maximum score of 25 for each extremity, totalling 50 for the lower limbs.
- In previous versions, a total motor score of 100 for all extremities was calculated. However, construct validity of the motor score as a measure of recovery following spinal cord injury and as an outcome measure for clinical trials is greater when upper extremity and lower extremity motor scores are scored independently and not summated together. Therefore, it is now recommended to consider upper extremity and lower extremity scores separately.
- The motor score provides a means of numerically documenting changes in motor function, but cannot be calculated if any required muscle function is "not testable."[3]
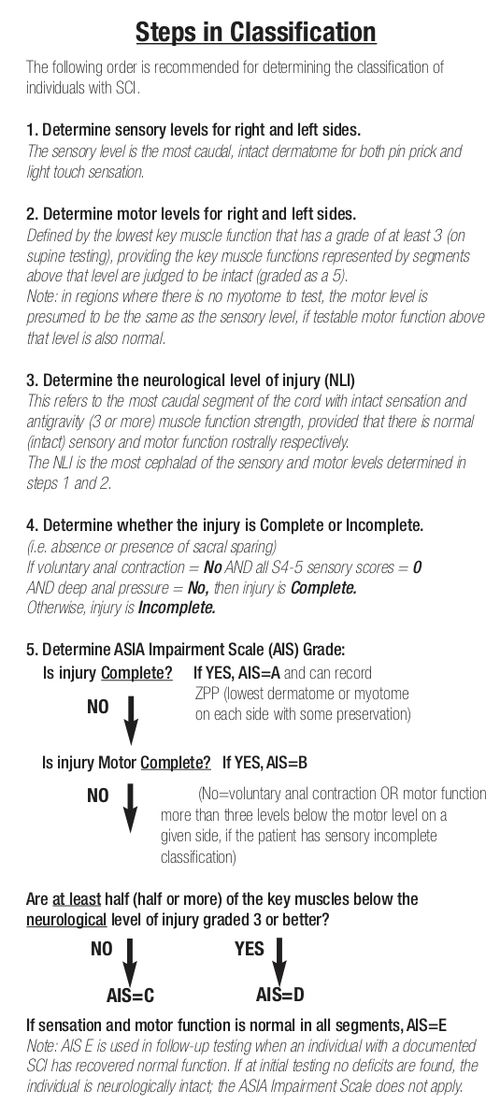
Determination of Neurological Level of Injury[edit | edit source]
The neurological level of injury is determined by identifying the most caudal segment of the spinal cord with intact sensation and antigravity muscle function strength (Grade 3 or more) on both sides of the body, provided that there is normal/intact sensory and motor function (Grade 5) rostrally.
- If there is a discrepancy between the most caudal intact section between the four possible levels of Right-Sensory Level, Left-Sensory Level, Right-Motor Level, or Left-Motor Level, the Neurological Level of Injury is considered the most cephalad segment of these four levels.[3]
ASIA Impairment Scale (AIS)[edit | edit source]
Spinal cord injuries are classified in general terms of being neurologically “complete” or “incomplete” based upon sacral sparing. Sacral sparing "refers to the presence of sensory or motor function in the most caudal sacral segments as determined by the examination (i.e. preservation of light touch or pin prick sensation at the S4-5 dermatome, DAP [deep anal pressure] or voluntary anal sphincter contraction)."[3]
Complete Injury: absence of sacral sparing i.e. no sensory and motor function at S4-5
Incomplete Injury: presence of sacral sparing i.e. partial preservation of sensory and/or motor function at S4-5
Sensory Incomplete: sacral sparing of sensory function
Motor Incomplete: sacral sparing of motor function or sacral sparing of sensory and motor function more than 3-levels below the level of injury
ASIA Impairment Scale (AIS)[edit | edit source]
| Grade | Type of Injury | Description of Injury |
|---|---|---|
| A | Complete | No sensory or motor function is preserved in sacral segments S4-S5, no sacral sparing |
| B | Sensory Incomplete | Sensory but not motor function is preserved below the neurological level and includes sacral segments S4-S5,
AND No motor function is preserved more than three levels below the motor level on either side of the body |
| C | Motor Incomplete | Motor function is preserved below the neurological level
AND More than half of the key muscle functions below the neurological level of injury have a muscle grade of less than 3 (Grades 0-2) |
| D | Motor Incomplete | Motor function is preserved below the neurological level
AND At least half (half or more) of the key muscle functions below the neurological level of injury have a muscle grade ≥ 3 |
| E | Normal | If sensation and motor function are graded as normal in all segments
AND the patient had prior SCI-related deficits *Individuals without a spinal cord injury do not receive an AIS Grade. |
| Information in the above table is adapted from the 2011 version of International Standards for Neurological Classification of Spinal Cord Injury.[3] | ||
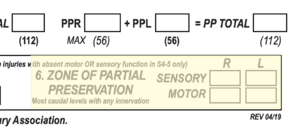
Zone of Partial Preservation[edit | edit source]
In previous versions, the zone of partial preservation (ZPP) was only determined for complete SCI (AIS A).[3] However, with the 2019 revision, the ZPP now applies to all cases regardless of the AIS grade.[2]
The zone of partial preservation refers to the dermatomes and myotomes caudal to the sensory or motor level that remain partially innervated. The extent of the sensory or motor ZPP is determined by the most caudal segment with some sensory or motor function respectively, and should be recorded for both right and left sides and for sensory and motor function.[3]
- Motor ZPP is recorded in incomplete injuries with absent VAC.
- Sensory ZPP is recorded in the absence of sensory function in S4-5 (light touch and pin-prick), as long as DAP is not present.
- In the presence of DAP, Sensory ZPP should be noted as “not applicable (NA)”.
- In the absence of DAP, sensory ZPP can be recorded if there is absence of light touch and pin-prick sensation at S4-5, while it should be noted as “not applicable (NA)” if there is presence of light touch or pin-prick sensation at S4-5.[2]
Steps in Classification[edit | edit source]
Psychometrics[edit | edit source]
Reliability and Validity[edit | edit source]
The International Standards for Neurological Classification of Spinal Cord Injury sensory and motor examinations are reliable when conducted by a trained examiner.[9] Both interrater and intrarater reliability were found to be excellent.[10][11] The correlation coefficients for both interrater and intrarater motor and sensory assessment are 0.90 or greater. This shows a high agreement between assessments. Incomplete injuries tend to have weaker interrater and intrarater correlations than complete injuries.[12]
Formal training in the administration of the International Standards for Neurological Classification of Spinal Cord Injury Standards has been shown to improve the accuracy of the examiner’s classification.[13]
The ASIA scale has strong prognostic values seen across multiple functional outcomes and may help predict recovery of autonomic functions such as bowel/bladder, cardiovascular, respiratory, and reproductive ability, and future ambulation potential.
Resources[edit | edit source]
Optional Technique Videos[edit | edit source]
Dermatome Testing Videos
Myotome Testing Videos
Upper limb
Lower Limb
International Standards for Neurological Classification of Spinal Cord Injury: Assessment Forms
- ASIA Impairment Scale: International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) Assessment Form
- ASIA Impairment Scale: Autonomic Standards Assessment Form
International Standards for Neurological Classification of Spinal Cord Injury: Sensory and Motor Guides
- ASIA Impairment Scale: Key Sensory Points
- ASIA Impairment Scale: Motor Exam Guide
ASIA E-Learning Centre InSTeP: International Standards
- To promote the teaching and competent use of the Standards, ASIA with contribution from the International Spinal Cord Society has developed the International Standards Training e-Learning Program or InSTeP.
ASIA E-Learning Centre ASTeP: Autonomic Anatomy & Function
- The goal of this training for the Autonomic Standards is to learn normal autonomic functions, understand the changes in autonomic functions following spinal cord injury (SCI) and use the Autonomic Assessment to document and classify remaining autonomic neurological function.
References[edit | edit source]
- ↑ Golestani A, Shobeiri P, Sadeghi-Naini M, Jazayeri SB, Maroufi SF, Ghodsi Z, Dabbagh Ohadi MA, Mohammadi E, Rahimi-Movaghar V, Ghodsi SM.Epidemiology of traumatic spinal cord injury in developing countries from 2009 to 2020: A systematic review and meta-analysis. Neuroepidemiology. 2022 May 5;56(4):219-39.
- ↑ 2.0 2.1 2.2 ASIA and ISCoS International Standards Committee. The 2019 revision of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)-What's new? Spinal Cord. 2019 Oct;57(10):815-817.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 Burns S, Biering-Sørensen F, Donovan W, Graves D, Jha A, Johansen M, Jones L, Krassioukov A, Kirshblum, Mulcahey MJ, Schmidt Read M, Waring W. International Standards for Neurological Classification of Spinal Cord Injury, Revised 2011. Top Spinal Cord Inj Rehabil 2012;18(1):85-99.
- ↑ Sandean D. Management of acute spinal cord injury: a summary of the evidence pertaining to the acute management, operative and non-operative management. World journal of orthopedics. 2020 Dec 12;11(12):573.
- ↑ 5.0 5.1 Docimo S, Diggs L, Crankshaw L, Lee Y, Vinces F. No evidence supporting the routine use of digital rectal examinations in trauma patients. Indian Journal of Surgery. 2015 Aug;77:265-9.
- ↑ Beeton G, Alter N, Zagales R, Wajeeh H, Elkbuli A. The benefits and clinical application of the digital rectal exam in trauma populations: Towards enhancing patient safety and quality outcomes. The American Journal of Emergency Medicine. 2022 Nov 8.
- ↑ Fernández-de Thomas RJ, De Jesus O. Thoracolumbar spine fracture. InStatPearls [Internet] 2021 Aug 30. StatPearls Publishing.
- ↑ Eli I, Lerner DP, Ghogawala Z. Acute traumatic spinal cord injury. Neurologic Clinics. 2021 May 1;39(2):471-88.
- ↑ Marino R, Jones L, Kirshblum S, Tal J, Dasgupta A. Reliability and repeatability of the motor and sensory examination of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med 2008;31(2)166-170.
- ↑ Clifton G, Donovan W, Dimitrijevic M et al. Omental transposition in chronic spinal cord injury. Spinal Cord 1996; 34:193–203.
- ↑ Savic G, Bergström EM, Frankel HL, Jamous MA, Jones PW. Inter-rater reliability of motor and sensory examinations performed according to American Spinal Injury Association standards. Spinal Cord. 2007;45(6):444-51.
- ↑ Roberts TT, Leonard GR, Cepela DJ. Classifications in brief: American spinal injury association (ASIA) impairment scale. 2017.
- ↑ Schuld C, Wiese J, Franz S, Putz C, Stierle I, Smoor I, Weidner N, EMSCI Study Group, Rupp RR. Effect of formal training in scaling, scoring and classification of the international standards for neurological classification of spinal cord injury. Spinal Cord 2013;51(4):282-8.